Health & fitness
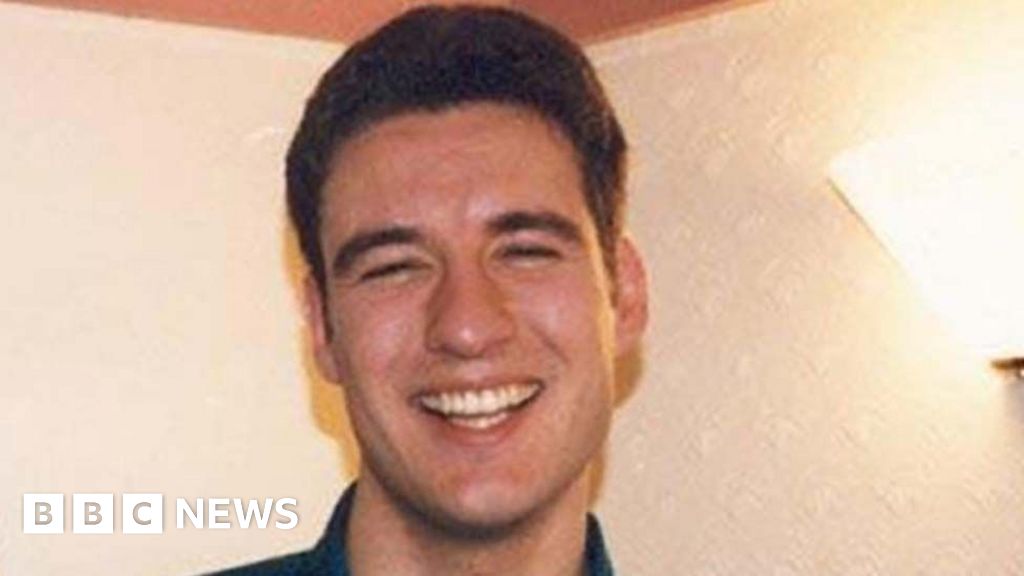
Man, 34, died of cancer after medics dismissed symptoms as ‘anxiety’ and told him to take more vitamin D inquest finds

A MAN who died of cancer just three days after he was first seen by a doctor may have been diagnosed earlier if it hadn’t been for Covid, an inquest ruled.
Oliver Philpott, 34, called his GP practice at least six times during the Covid lockdown complaining of long-term fatigue, anxiety and back pain.
But due to pandemic rules restricting the number of face-to-face GP appointments he was repeatedly assessed over the phone instead.
Four months after he first reported symptoms Mr Philpott finally saw his GP at the surgery.
He died three days later.
A post mortem later found the 34-year-old had a large 20cm tumour wrapped around his heart and lungs.
The aggressive cancer had infiltrated his right lung and had eventually caused pulmonary emboli which led to a cardiac arrest that killed him.
In a double family tragedy, his father, Anthony – wracked by guilt and grief over the death of his son – killed himself.
An inquest into Oliver’s death in Hastings heard a GP triage system had been introduced by the NHS during the pandemic to restrict face-to-face appointments to prevent the spread of the disease.
As a result a triage system had been introduced at Oliver’s doctors’ practice, Rye Medical Centre, East Sussex.
Fiona King, senior coroner for East Sussex, said: “This is not a case where I can find a failure to have a system in place.
“However the emergency Covid triage system may have had a deleterious affect in Oliver’s prospects of earlier diagnosis and treatment.”
After the inquest his sister, Victoria, said: “The failure to diagnose Oliver and the inadequate systems put in place highlight how ill-prepared we were for the pandemic.”
Mr Philpott, who had only rarely seen a doctor, first called the surgery in February 2021 complaining of long-term fatigue.
Dr George Taggart assessed him over the phone and ordered blood tests which showed he had a slightly elevated white blood cell count – normally associated with the body fighting an infection or inflammation – and low Vitamin D levels.
Mr Philpott was given the all clear and told to take a Vitamin D supplement.
However on April 29 Mr Philpott called the surgery again where he was triaged by paramedic practitioner, Jamie Clarke.
Mr Philpott told the paramedic the back pain he had suffered since January was not improving.
He said he had given up weight-lifting in the the gym as a result but was continuing to feel tired and anxious.
Mr Clarke prescribed painkiller Naproxen and referred the builder and to physiotherapist, Nicola Bamford, who carried out a phone assessment on April 30.
On May 7 he saw the physiotherapist in a face-to-face appointment who felt he was able to carry out the exercise assessments with ease.
As a result she deduced his pain was muscular-skeletal and gave him breathing exercises to deal with his anxiety.
The inquest heard that despite telling the physiotherapist his pain levels were sometimes eight out of 10 she did not refer him back to the GPs.
However Mr Philpott called the medical centre again saying he was still struggling with bad back pain, was having difficulty sleeping and continued to be anxious.
On May 11 Mr Philpott had a telephone consultation with Dr Warner, the inquest heard, where he told her about his symptoms.
Without seeing him in person she prescribed an anti-depressant to help with his anxiety.
On June 2 he phoned back again and told the paramedic practitioner he still had constant back pain but now had swelling in his arms and legs.
He also said he was suffering from fatigue, wasn’t able to sleep and was still suffering anxiety as a result.
Mr Philpott was told to call back if the pain in his back dramatically increased and the call ended.
On June 11 his desperately worried father, Anthony, called Rye Medical Centre and said he was seriously worried about his son.
He said his son was very ill and had lost a huge amount of weight and couldn’t get out bed.
However Dr Taggart told him he could not discuss his son’s case without prior permission being granted by the 34-year-old.
On June 15 his sister Victoria succeeded in obtaining an appointment at the surgery and pushed her poorly brother into the consulting room in a wheelchair.
Dr Warner told the inquest: “He was probably one of the most unwell people I have seen come into a GP surgery.
“No previous history given earlier that would have told us he was so unwell.”
She referred Mr Philpott to A&E and he was immediately admitted to Conquest Hospital, Hastings, before being transferred to intensive care where he died three days later.
Dr Warner told the family Covid had limited the number of patients the surgery could see and they had introduced through a triage system to assess patients.
Victoria Philpott said: “Well then, it didn’t work.”
Dr Warner said if Mr Philpott had reported his symptoms now then he would have been given a face-to-face appointment.
Recording a narrative conclusion coroner Mrs King said: “Oliver died of complications of a very rare and very aggressive cancer which caused strangulation of the blood flow to his heart and lungs.
“An opportunity to diagnose his illness by way of a face-to-face examination by the GP did not occur due to national NHS Covid restrictions requiring triaging of patients and telephone appointments.”
After the inquest hearing his sister, Victoria, said: “Oliver may not have died from Covid but the pandemic effectively killed him.
“The inquest heard he probably would have been seen earlier but for the Covid triage system which failed him.
“We don’t blame anyone but it shows how ill-prepared we were for the pandemic.
“Oliver isn’t the only person to die as a result of this lack of effective pandemic planning but I just hope that by highlighting his case some good can come of it and improve how we respond in the future.”
Womens Workouts
Low Impact 30 minute cardio workout- Beginner/intermediate

https://teambodyproject.com
Transform your body in just 10 weeks and take part in the entire Body Project system. Start your Body Project TODAY!
Or simply come and join the conversation at http://www.facebook.com/bodyprojectso…
In this 30 minute cardio workout, I (Daniel) take you through a number of interval drills to raise your heart rate, burn calories and release those feel good hormones.
Comment below to let us know how you get on!
This low impact cardio workout includes a warm up and a cool down before and after the exercise routine, we advise you follow both for safety and best practise.
This beginner routine is in our cardio range – we also provide Personal Training (resistance), Pilates and Yoga workouts.
Enjoy the workout!
Exercise disclaimer –
As with any physical activity, before beginning any fitness regime, you must consult with your health care professional to ensure that you are mindful of your current health and any restrictions that are appropriate for you.
You should seek medical attention immediately if there are any unanticipated changes to your physical condition at any time.
None of the information contained within this Website or on our videos is intended to be used as medical advice and the Website is not intended to be used to diagnose, treat, cure or prevent any medical condition (including any mental health conditions) or for any therapeutic purposes.
Before relying on the information on this Website, it is your responsibility to carefully evaluate the accuracy and relevance of the information for their purposes and obtain appropriate professional medical advice.
Always consult a qualified medical professional if you have any questions concerning your medical condition or injury.
source
Womens Workouts
#malaikaarora 's post workout glow is making us feel like hitting the gym soon! 😉 #shorts

#malaikaarora ‘s post workout glow is making us feel like hitting the gym soon! 😉 #shorts
source
Womens Workouts
30 MIN FULL BODY WORKOUT No Equipment (From the MadFit App)

DOWNLOAD YOUR FREE TRIAL HERE : https://madfit.app.link/e/store
Do this 30 minute FULL BODY WORKOUT from INSIDE THE MADFIT APP! This is an exclusive workout from the 12 week Full Body program!
#MadFit #Workout #Fitness
INSTAGRAM: @themadfitapp @madfit.ig
source
Health & fitness
Mum-of-two, 43, died at home after her heart stopped while waiting 2 hours for an ambulance

A MUM-of-two died from a heart attack while waiting for an ambulance for more than two hours, a court has heard.
Julie Hurn, 43, died at her home in Attleborough, Norfolk on June 25, 2022, having suffered a myocardial infarction – a blood clot stopped her heart.
She called 999 after experiencing chest pains.
An inquest into her death at Norfolk Coroner’s Court heard that it was likely she would have survived if she had received immediate treatment.
Rajesh Logasundaram, who carried out a post mortem examination, said: “An earlier 999 call would have made a significant difference to her chances of survival.”
The court heard she had originally phoned for an ambulance at 3.26pm after she experienced chest paints, with her call given category two status.
Read more on heart attacks
Serious conditions such as strokes or chest pain which may require rapid assessment and urgent transport are classed as category two.
Julie called again around an hour later after she began vomiting, but it was not until shortly before 5pm that her call was escalated.
A neighbour had phoned again to say she had gone into cardiac arrest – meaning her heart stopped beating – and paramedics arrived at 5.14pm.
Mrs Hurn, who worked as a contracts manager for Norfolk County Council, died at 5.48pm, 142 minutes after her first call to emergency services.
It was revealed in court that when her original call was made, 50 of the region’s ambulances were stranded outside Norfolk’s three main hospitals.
The incident happened during a “black surge”, a phrase used to describe a period of acute demand on emergency services and acute hospitals.
Chris Hewitson, a patient safety specialist officer at the East of England Ambulance Service Trust, said Mrs Hurn’s initial call was correctly categorised.
But at that time there were also 50 outstanding calls with the same priority level.
He added that there were 19 ambulances stranded outside of the Norfolk and Norwich University Hospital alone.
Yvonne Blake, area coroner for Norfolk, said: “The medical evidence we have heard so far is that if she had a cardiac arrest and either received immediate treatment or was in hospital, that given her age it is more likely than not that she would have survived.”
On Monday, Prof Saul Myerson, a consultant cardiologist based at the University of Oxford, said at the inquest that a faster response would have improved her chances.
Subtle signs of a heart attack
A HEART attack is when the supply of the blood to the heart is suddenly blocked.
It is a medical emergency and needs to be treated right away.
Around 100,000 people are admitted to hospital due to heart attacks every year in the UK, according to the British Heart Foundation.
That’s 290 each day, or one every five minutes.
Some symptoms, like chest pain, shortness of breath and feeling lightheaded or dizzy, can be fairly obvious.
But the signs aren’t always so blatant, the NHS warns. Other more subtle symptoms of a heart attack include:
- Pain in other parts of the body (it can feel as if the pain is spreading from your chest to your arms, jaw, neck, back and stomach)
- Sweating
- Feeling sick
- Vomiting
- An overwhelming feeling of anxiety (similar to a panic attack)
- Weakness or fatigue
- Coughing
- Wheezing
A heart attack and cardiac arrest are similar, but not the same.
A cardiac arrest is when the heart stops pumping blood around the body.
He said that while was unlikely her heart attack would have been prevented, had she been in hospital when it occurred her survival chances would have been better.
In a statement read to the court, her brother Gary Hambling said: “As a family we believe the NHS has let us down.
“The time taken to get an ambulance to her was unacceptable.”
Clare Gooch, a medical negligence lawyer from Switalskis, who is representing the family, said “This has been an incredibly difficult time for Mrs Hurn’s family who are still coming to terms with their loss.
“They now hope this inquest will help to provide some further insight into the circumstances leading up to her death.”
The inquest continues.
Symptoms of a cardiac arrest
A cardiac arrest is when your heart suddenly stops pumping blood around your body.
It’s sometimes mistaken for a heart attack but it’s different.
A cardiac arrest is an emergency that usually happens without warning.
If someone is in cardiac arrest, they collapse suddenly and:
- Will be unconscious
- Unresponsive, and
- Not breathing or not breathing normally – this may mean they’re making gasping noises.
Without immediate treatment, the person will die.
If you see someone having a cardiac arrest, phone 999 immediately and start CPR.
Source: British Heart Foundation
Health & fitness
Catching Covid doubles your risk of heart attack or stroke for the next THREE years, scientists warn
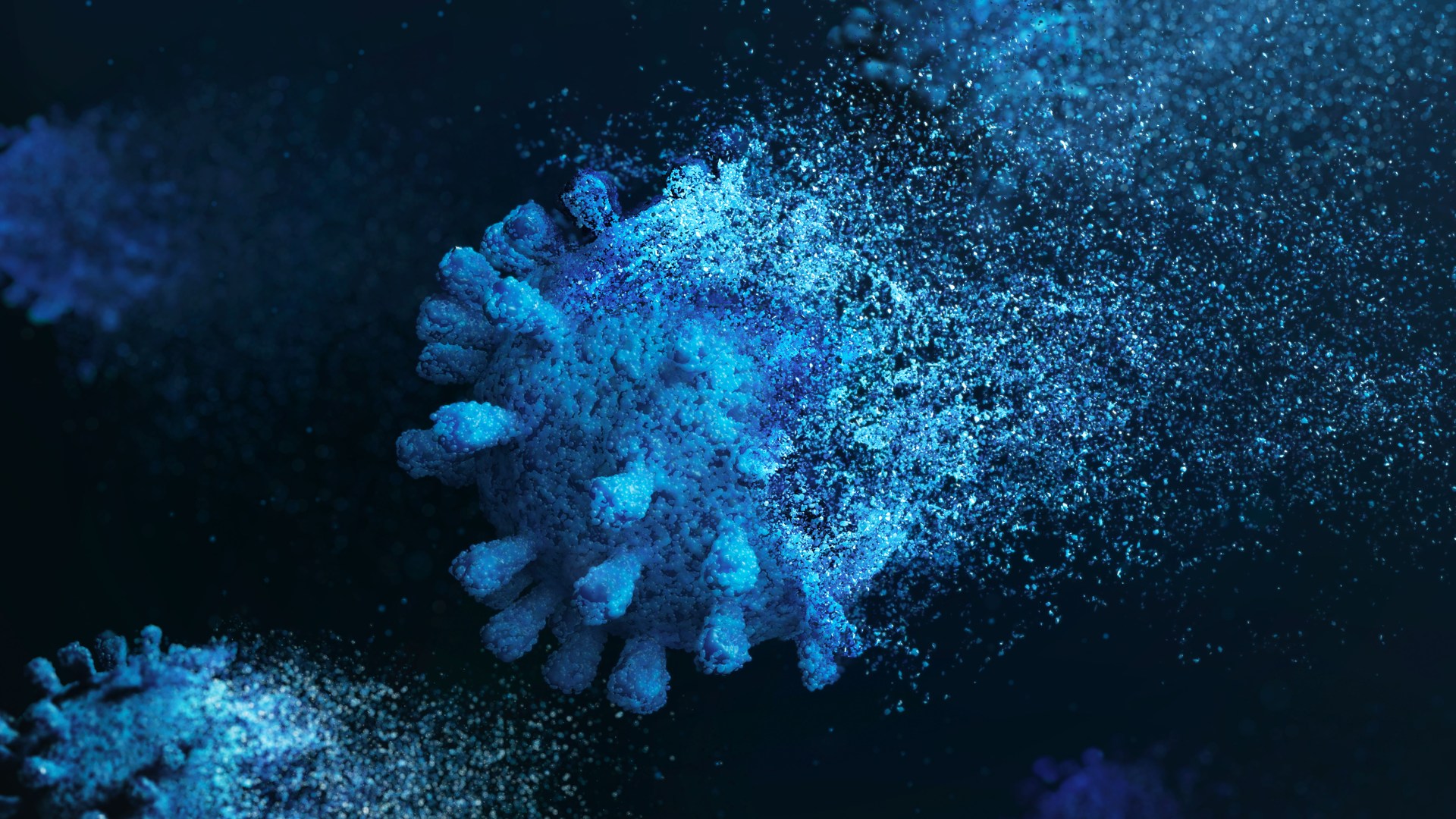
COVID doubles the risk of a heart attack, stroke or dying up to three years later, a new study warns.
The danger is even higher among people with blood types A, B or AB who were infected with the virus compared to those with type O, say scientists.
They reviewed data from more than 10,000 adults aged over 50, including around 8,000 who tested positive for Covid-19 from February 1 to December 31, 2020, and about 2,000 who tested positive for the virus in hospital in 2020.
A group of more than 200,000 adults who had no history of Covid infection during the same time frame and who were also taking part in the ongoing UK Biobank study were reviewed for comparison.
None of the participants were vaccinated at the time of infection because Covid-19 jabs were not yet available.
Researchers found that adults who had mild to severe Covid were more likely to have suffered a heart attack, stroke or died during the following three years.
The elevated risk of heart attack, stroke or death linked to Covid-19 infection was comparable to cardiovascular risk factors such as type 2 diabetes, peripheral artery disease and cardiovascular disease, according to the findings.
The study, published in the journal Arteriosclerosis Thrombosis and Vascular Biology, also found that having a non-O blood type was associated with an increased risk of a heart attack, stroke or death among those who were infected by Covid.
The American research team say their findings suggest that people infected with Covid might benefit from cardiovascular disease prevention treatments to lower the risk of a heart attack or stroke.
Study lead author James Hilser, of the University of Southern California Keck School of Medicine, Los Angeles, said: “We found a long-term cardiovascular health risk associated with Covid, especially among people with more severe Covid-19 cases that required hospitalisation.
“This increased risk of heart attack and stroke continued three years after Covid-19 infection.
“Remarkably, in some cases, the increased risk was almost as high as having a known cardiovascular risk factor such as type 2 diabetes or peripheral artery disease.”
Previous research has shown that Covid-19 increases the risk of serious cardiovascular complications within the first month after infection.
The new study examined how long the increased risk lasted and whether it subsided after recovering.
Researchers found that, during the near three-year follow-up period, the risk of a heart attack, stroke and death was more than double among adults who had Covid-19.
This risk was nearly four times greater among adults hospitalised with Covid-19, compared with those never infected with the virus.
People hospitalised with Covid, who didn’t have cardiovascular disease or type 2 diabetes, had a 21 per cent greater risk of a heart attack, stroke or dying compared to people with cardiovascular disease who didn’t get the virus.
The researchers also found a “significant” genetic interaction among the non-O blood types and hospitalisation for Covid.
Who can get an NHS Covid jab this autumn?

THE NHS has started offering autumn Covid boosters to the most vulnerable.
Many pharmacies also now sell the Covid jab privately.
Can I get it?
The following groups can have an NHS Covid booster between 3 October and 20 December:
- over-65s
- people aged between six months and 64 years with health conditions that make them more vulnerable, including pregnant women
- people living in care homes for older people
- frontline NHS and social care workers,and those working in care homes for older people
The NHS has already contacted more than 11 million people, but those who qualify for the jab can also book their own appointments via the NHS App,, GPs, pharmacies, drop-in clinics,or by calling 119.
Anyone also entitled to the flu jab will be offered this at the same time.
Patients who are also entitled to the respiratory syncytial virus (RSV) vaccine, will not usually be given it at the same time as a flu or Covid jab.
However, pregnant women can have the RSV vaccine at the same time as the Covid jab.
People with severe Covid-19 infections had an increased risk of heart attack and stroke, but that risk was even higher in people who had non-O blood types.
The risk of heart attack and stroke was around 65 per cent higher in adults with blood types A, B or AB compared to those who had type O blood.
‘Explains the rise in heart disease’
Study co-senior author Professor Stanley Hazen, chair of cardiovascular and metabolic sciences at Cleveland Clinic’s Lerner Research Institute, said: “Worldwide, over a billion people have already experienced Covid-19 infection.
“The findings reported are not a small effect in a small subgroup.
“The results included nearly a quarter million people and point to a finding of global health care importance that may translate into an explanation for a rise in cardiovascular disease around the world.”
Study co-senior study author Professor Hooman Allayee, also of the University of Southern California Keck School of Medicine, said: “The results of our study highlight the long-term cardiovascular effects of Covid-19 infection.
“Given the increased risk of heart attack, stroke and death, the question is whether or not severe Covid-19 should be considered as another risk factor for cardiovascular disease, much like Type 2 diabetes or peripheral artery disease, where treatment focused on cardiovascular disease prevention may be valuable.
“The results suggest that people with prior Covid infection may benefit from preventive care for cardiovascular disease.”
Professor Sandeep Das, co-chair of the American Heart Association, said of the findings: “They show that something located close to the genetic home of ABO blood type is associated with different degrees of susceptibility to Covid.”
He added: “This is really fascinating, and I look forward to seeing scientists tease out what the specific pathway may be.”
Womens Workouts
The Only 3 Exercises You Need for a Complete Glute Workout

@stalinkeviciute is back to get her glutes crushed by Dr. Mike and @JAREDFEATHERRP ‘s favorite glute exercises.
The UPDATED RP HYPERTROPHY APP: https://rpstrength.com/rphypeapp
Become an RP channel member and get instant access to over 200 videos of exclusive in-depth training and advanced science content! ➡️https://www.youtube.com/channel/UCfQgsKhHjSyRLOp9mnffqVg/join
0:00 Laura Intro
1:32 Reverse Lunge
8:07 Squat
14:25 Hamstring Lean
20:10 Contemplating Life & Wrap Up
source
-

 Womens Workouts2 weeks ago
Womens Workouts2 weeks ago3 Day Full Body Women’s Dumbbell Only Workout
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoHow to unsnarl a tangle of threads, according to physics
-
 Science & Environment3 weeks ago
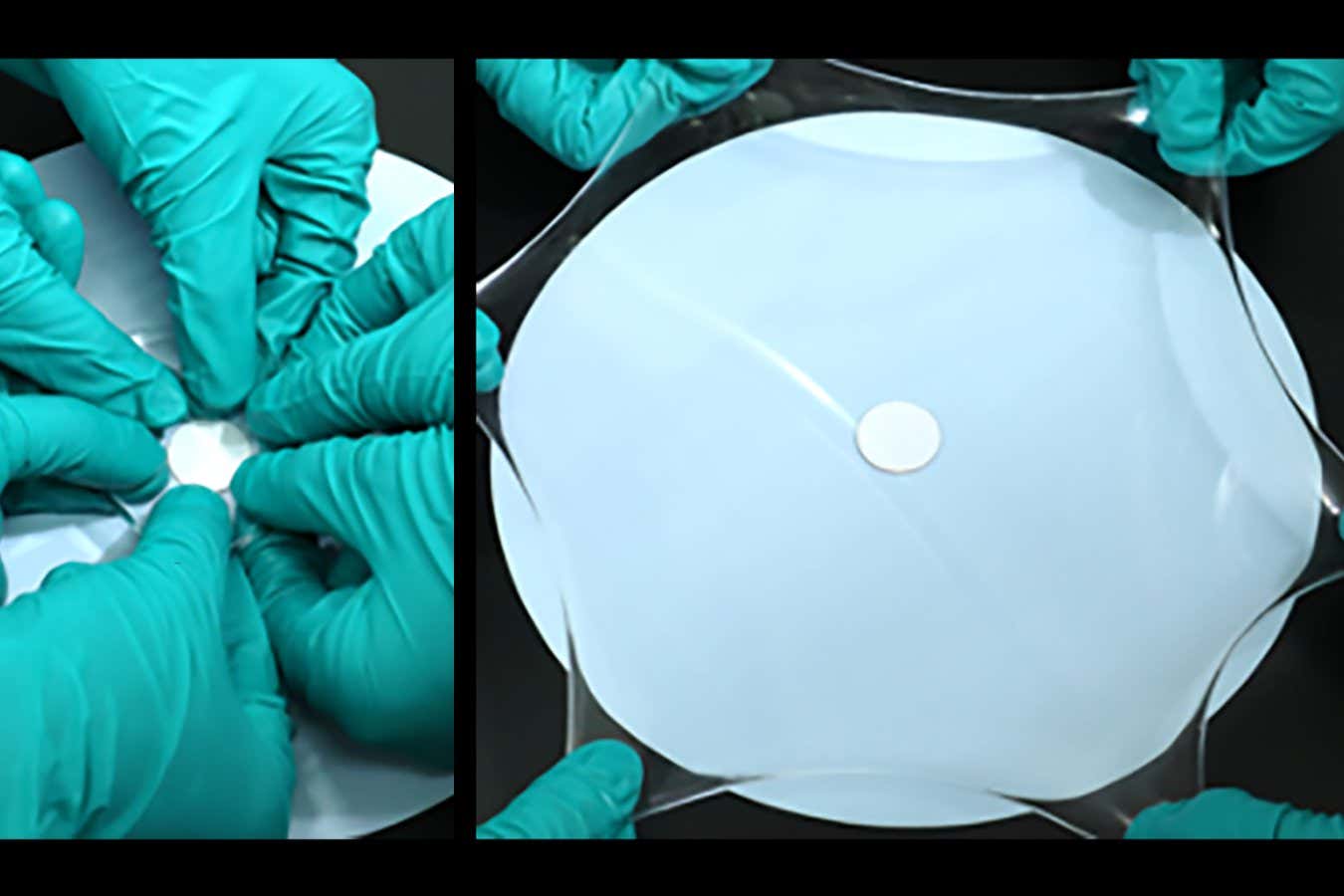
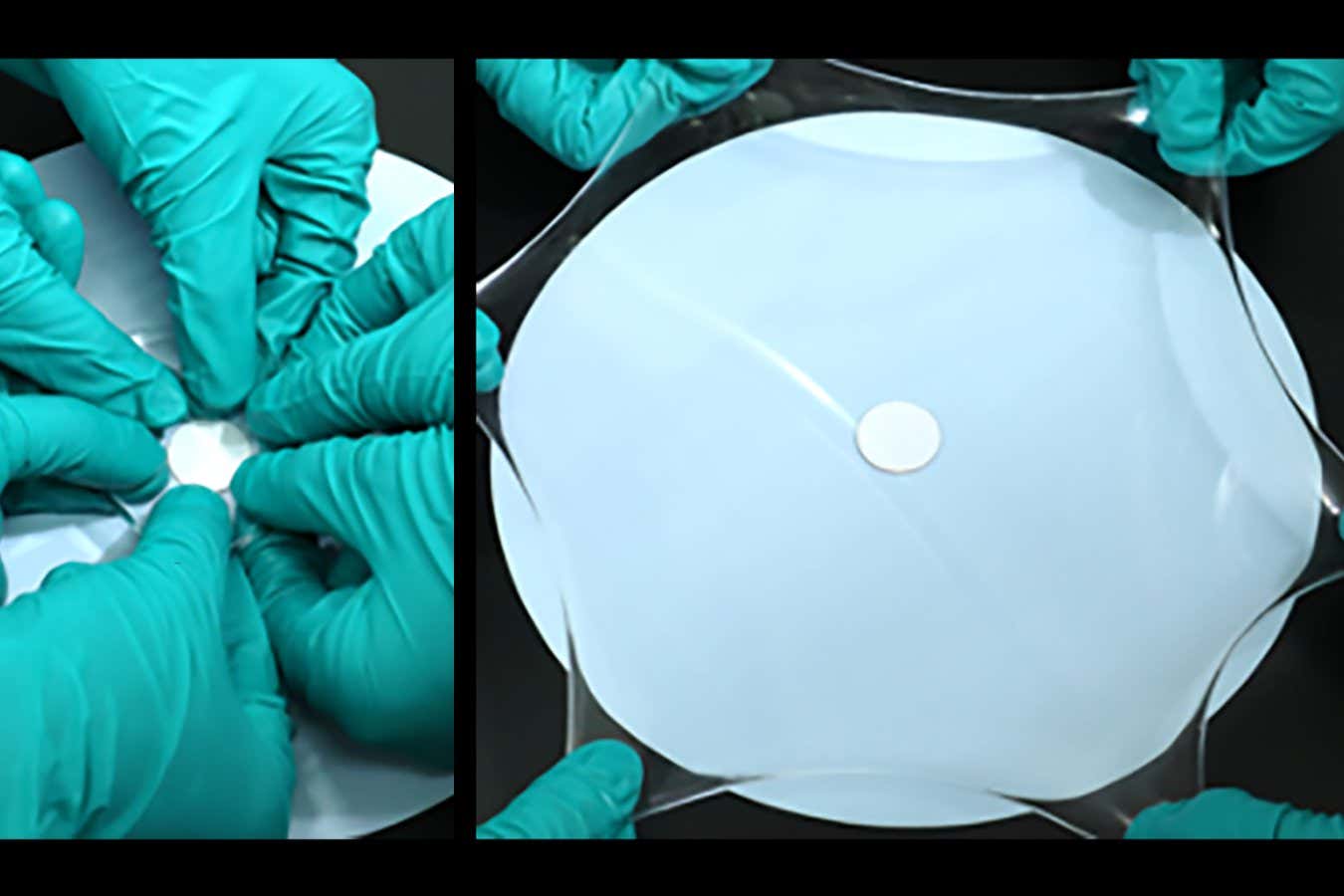
Science & Environment3 weeks agoHyperelastic gel is one of the stretchiest materials known to science
-

 Technology3 weeks ago
Technology3 weeks agoWould-be reality TV contestants ‘not looking real’
-

 Science & Environment3 weeks ago
Science & Environment3 weeks ago‘Running of the bulls’ festival crowds move like charged particles
-

 Science & Environment3 weeks ago
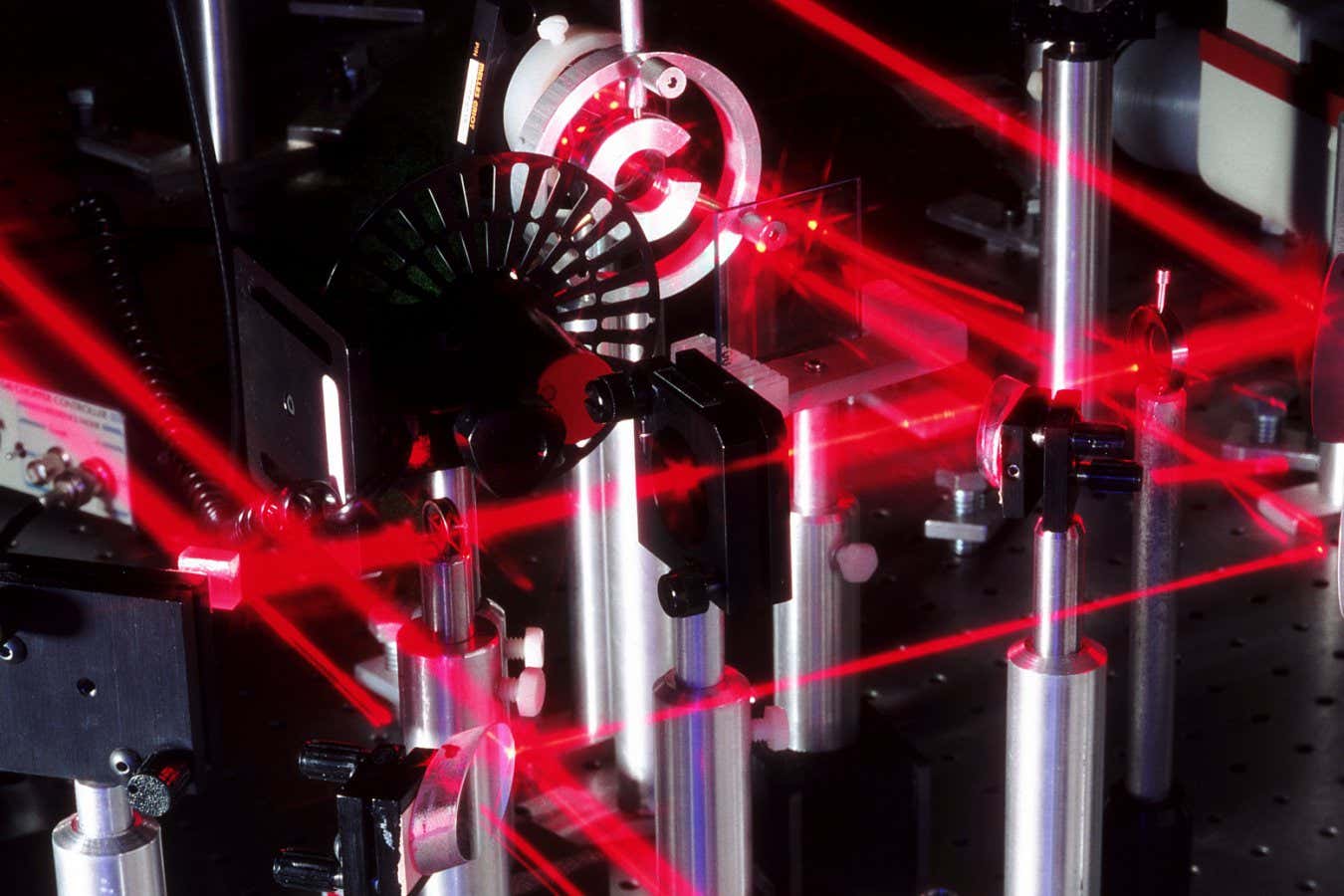
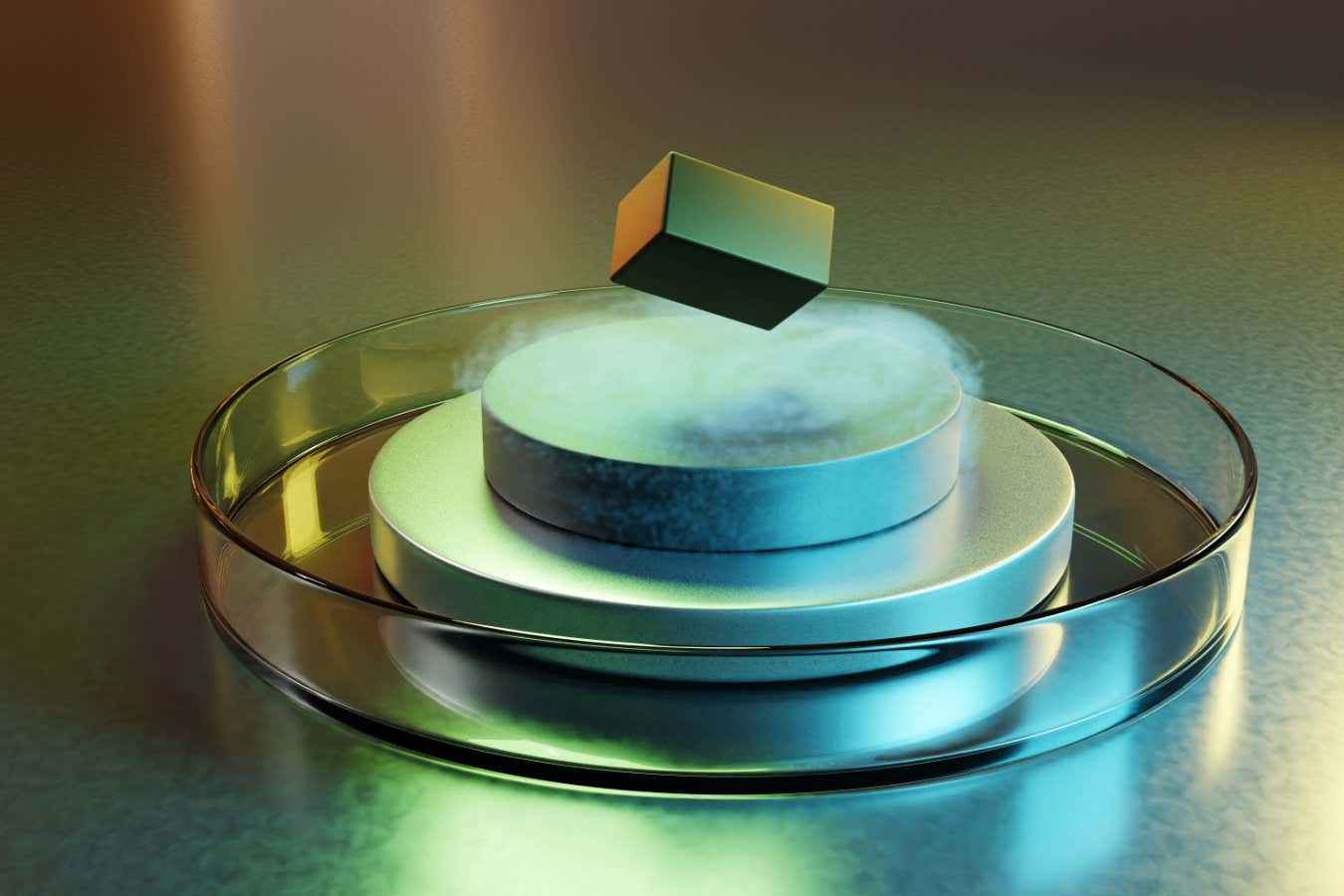
Science & Environment3 weeks agoMaxwell’s demon charges quantum batteries inside of a quantum computer
-

 News2 weeks ago
News2 weeks agoOur millionaire neighbour blocks us from using public footpath & screams at us in street.. it’s like living in a WARZONE – WordupNews
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoSunlight-trapping device can generate temperatures over 1000°C
-
News3 weeks ago
the pick of new debut fiction
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoHow to wrap your mind around the real multiverse
-
 Science & Environment3 weeks ago
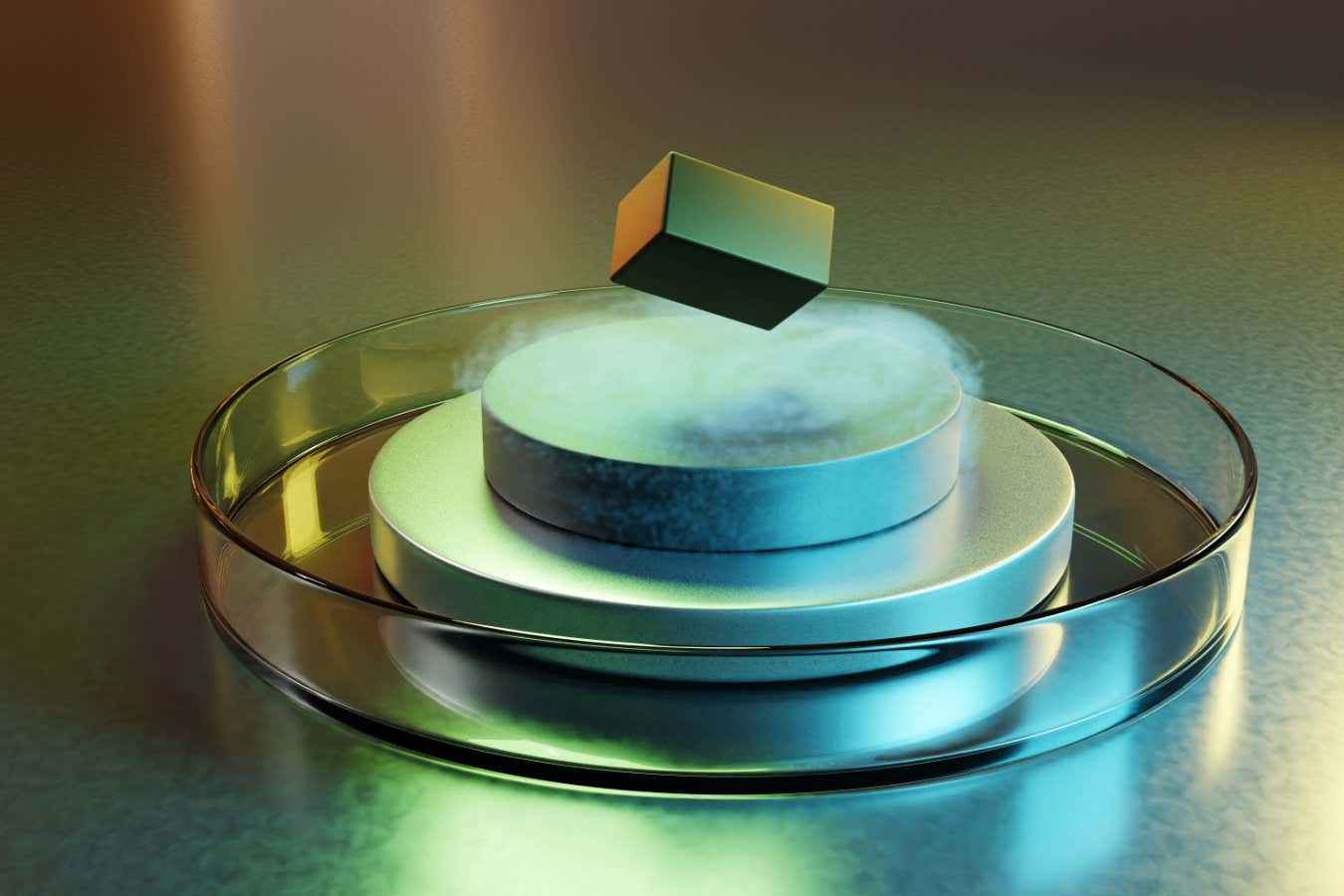
Science & Environment3 weeks agoQuantum ‘supersolid’ matter stirred using magnets
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoLiquid crystals could improve quantum communication devices
-

 Science & Environment3 weeks ago
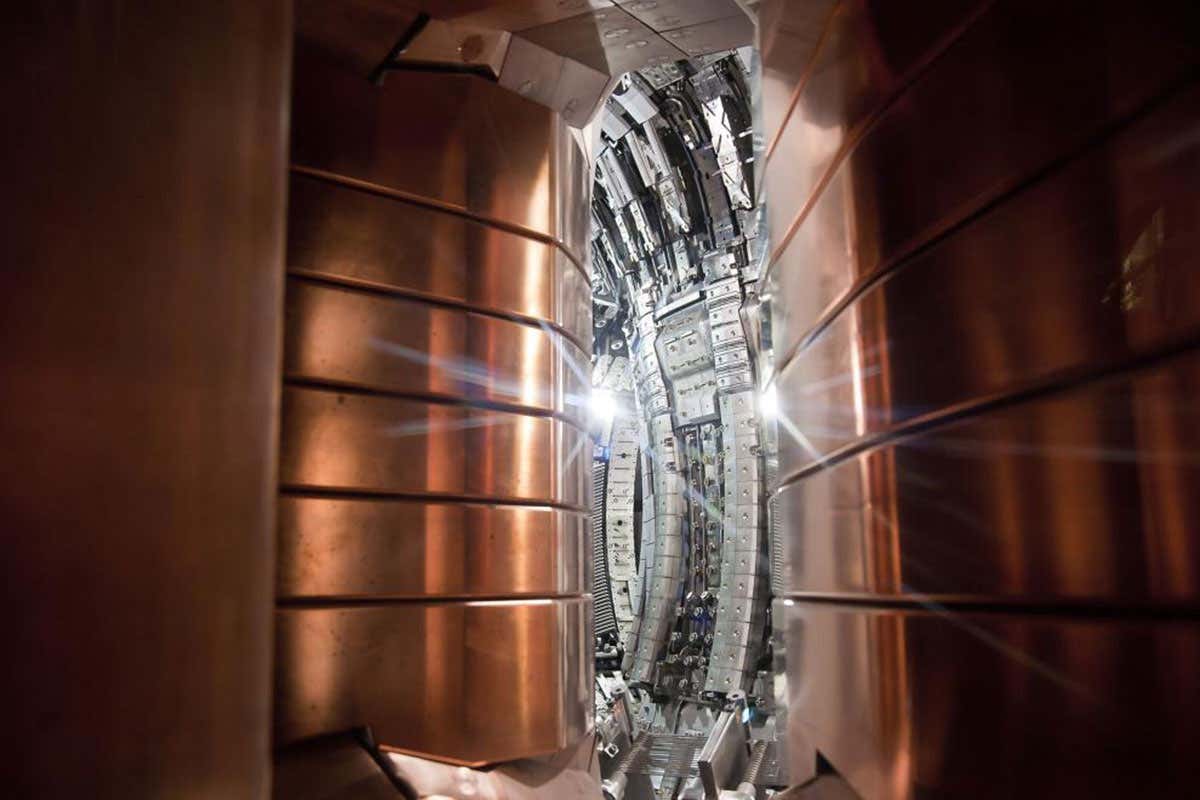
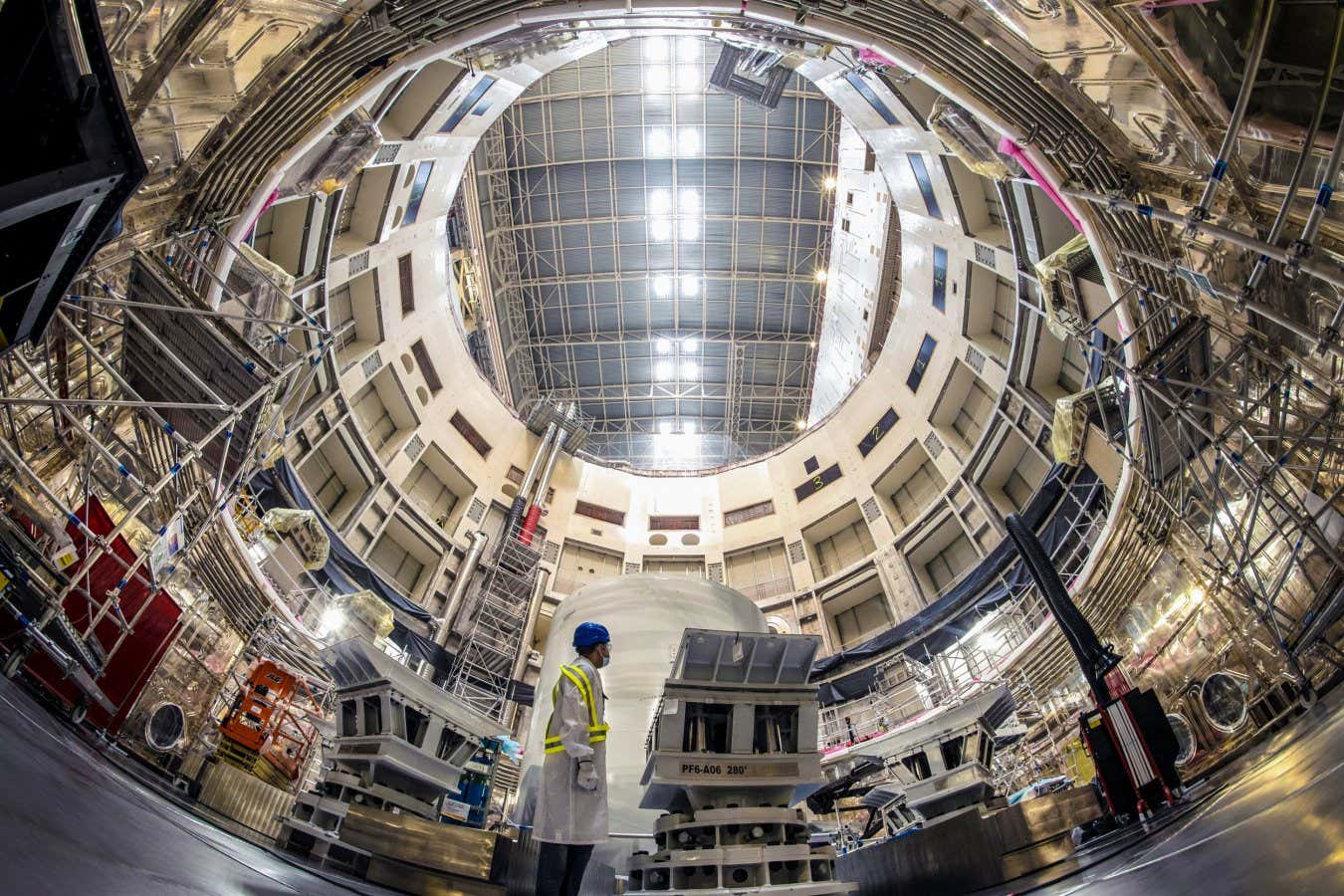
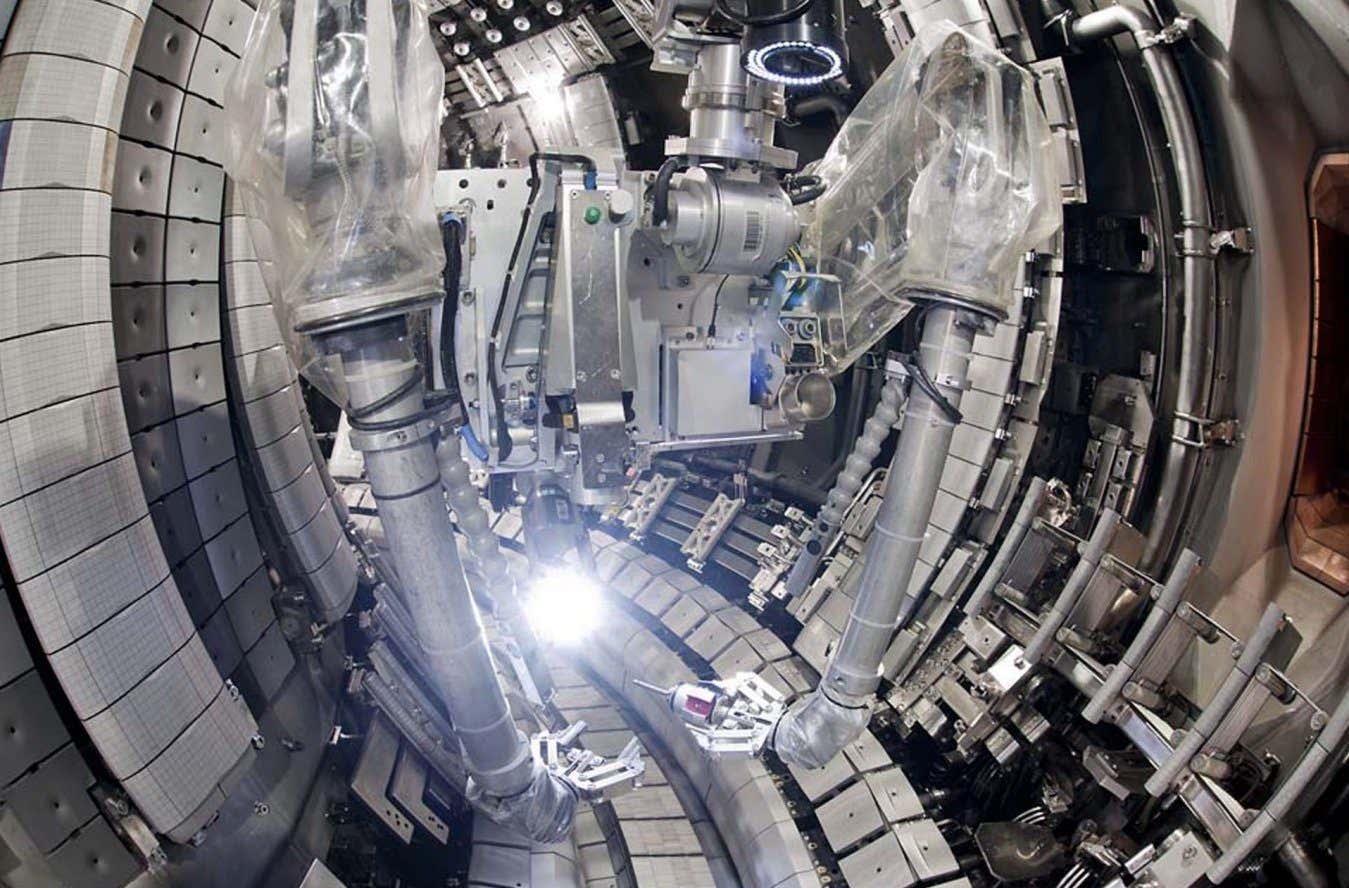
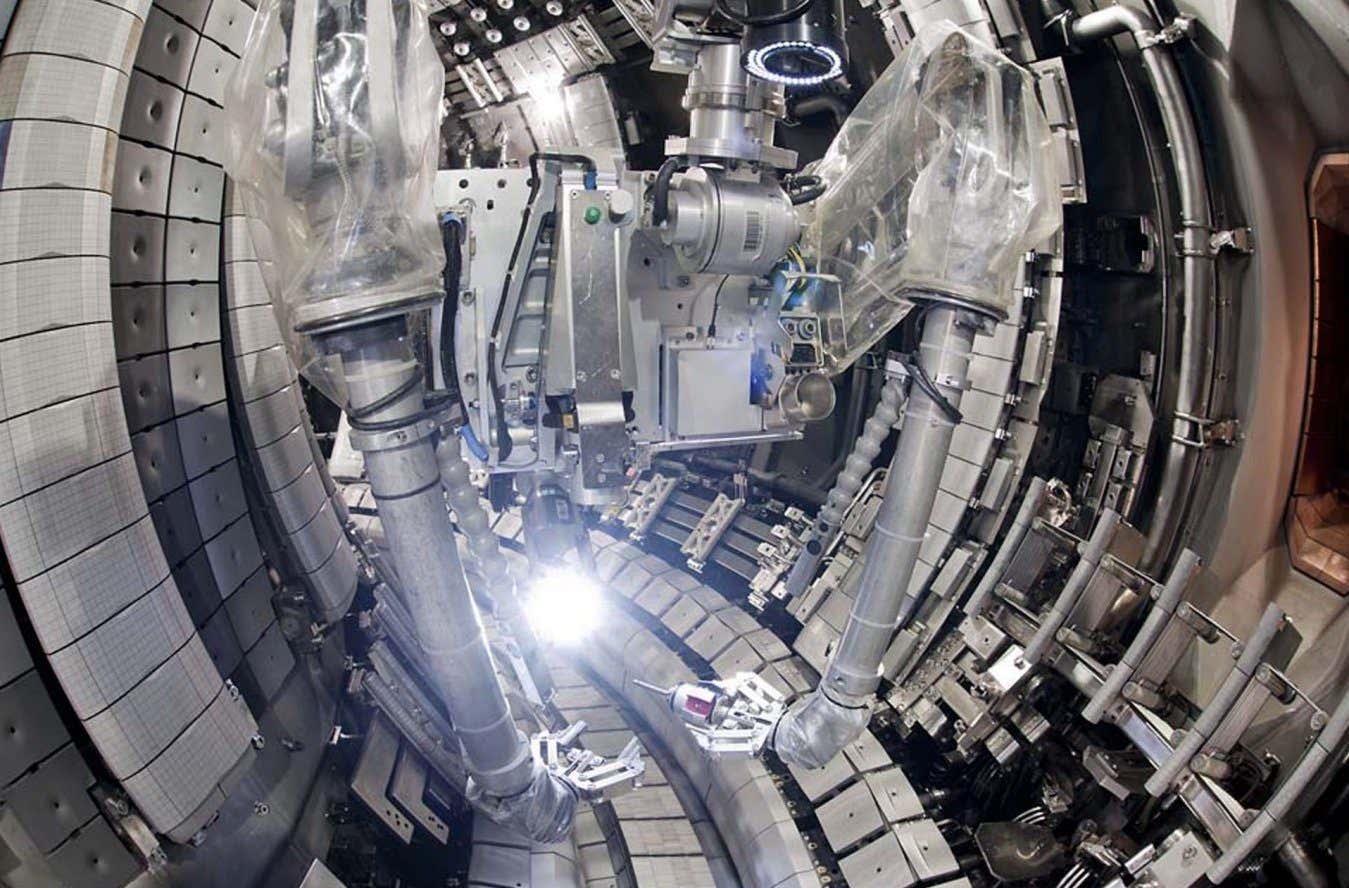
Science & Environment3 weeks agoITER: Is the world’s biggest fusion experiment dead after new delay to 2035?
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoQuantum forces used to automatically assemble tiny device
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoPhysicists are grappling with their own reproducibility crisis
-
 Science & Environment3 weeks ago
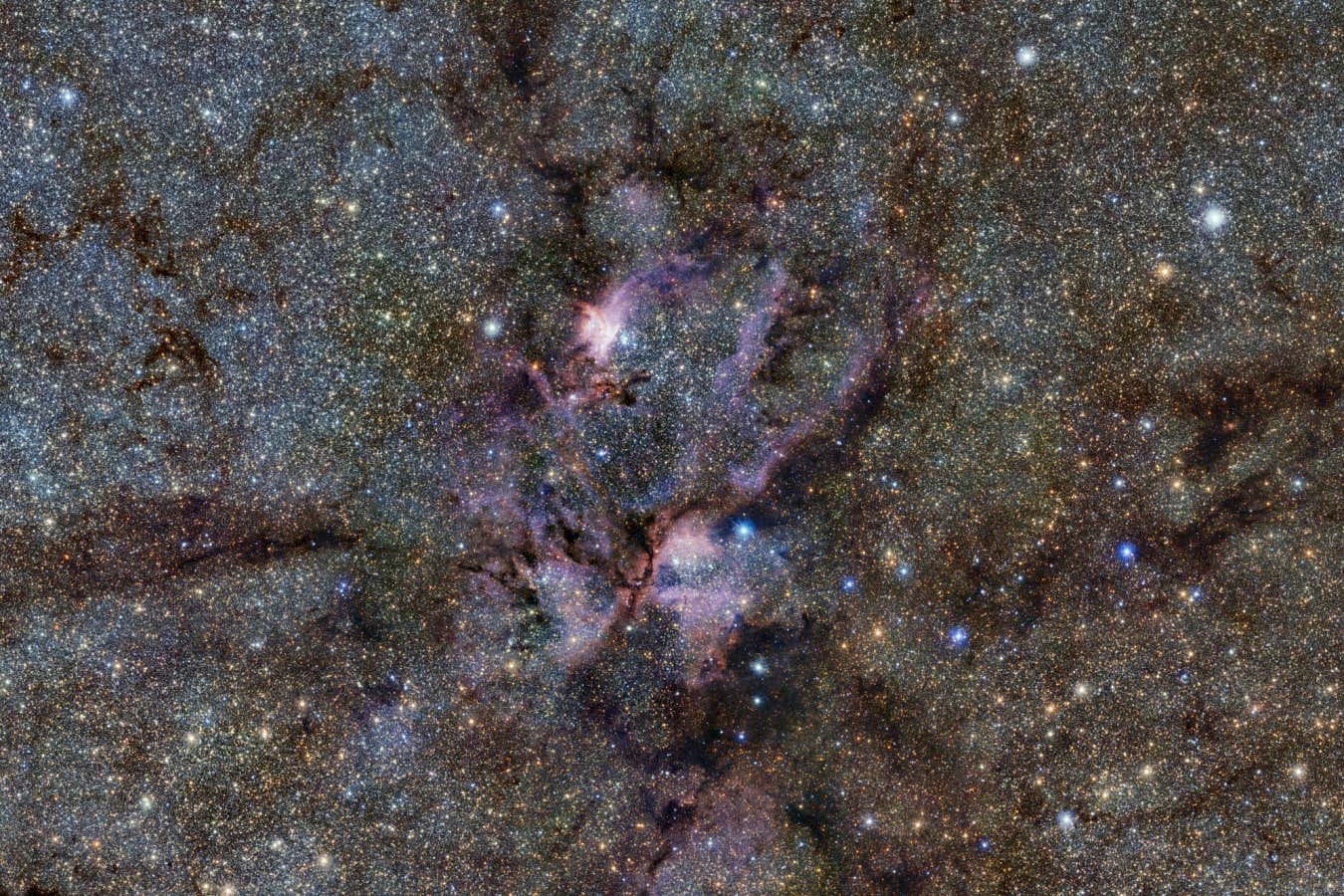
Science & Environment3 weeks agoWhy this is a golden age for life to thrive across the universe
-

 News3 weeks ago
News3 weeks agoYou’re a Hypocrite, And So Am I
-

 Sport3 weeks ago
Sport3 weeks agoJoshua vs Dubois: Chris Eubank Jr says ‘AJ’ could beat Tyson Fury and any other heavyweight in the world
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoTime travel sci-fi novel is a rip-roaringly good thought experiment
-
 Science & Environment3 weeks ago
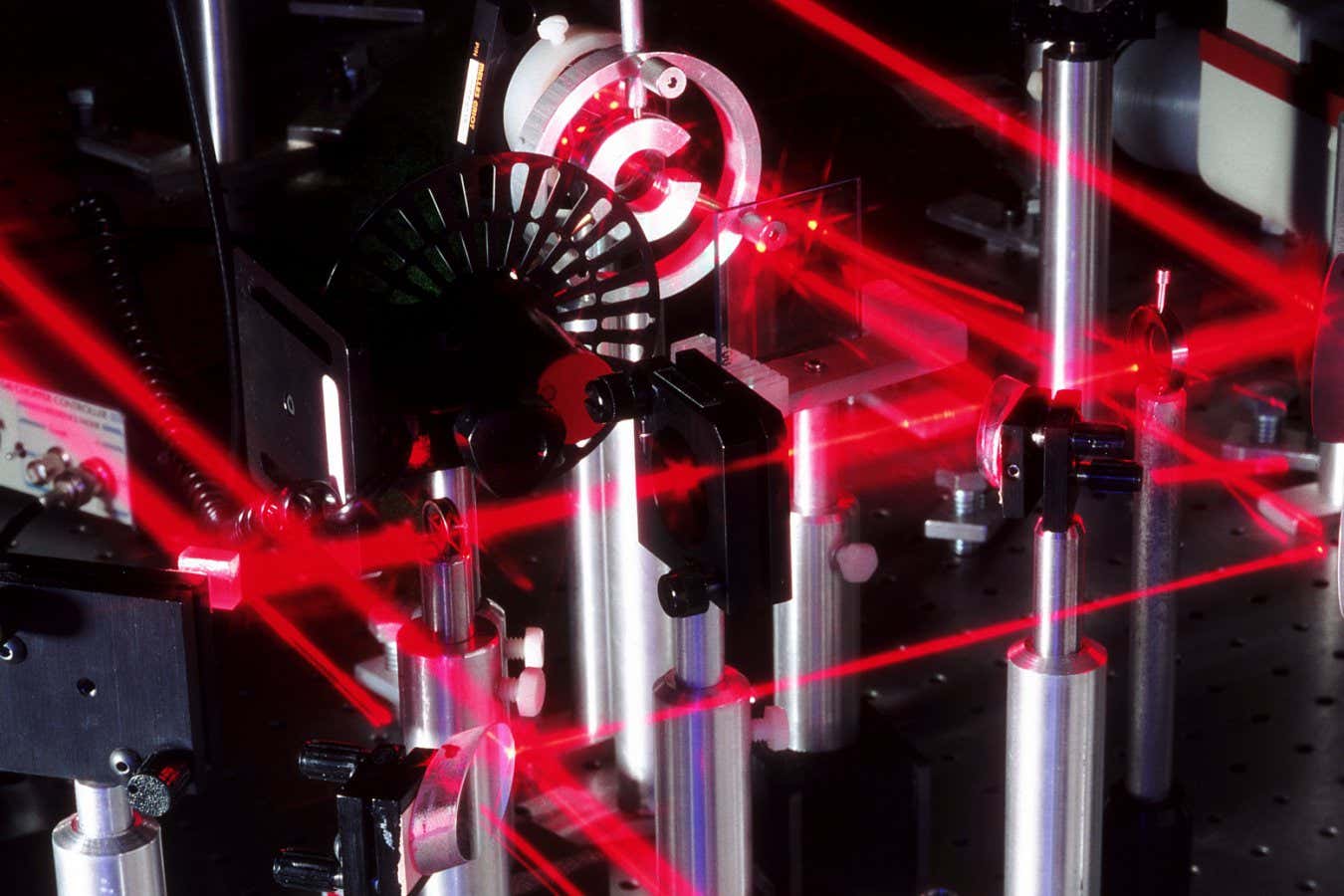
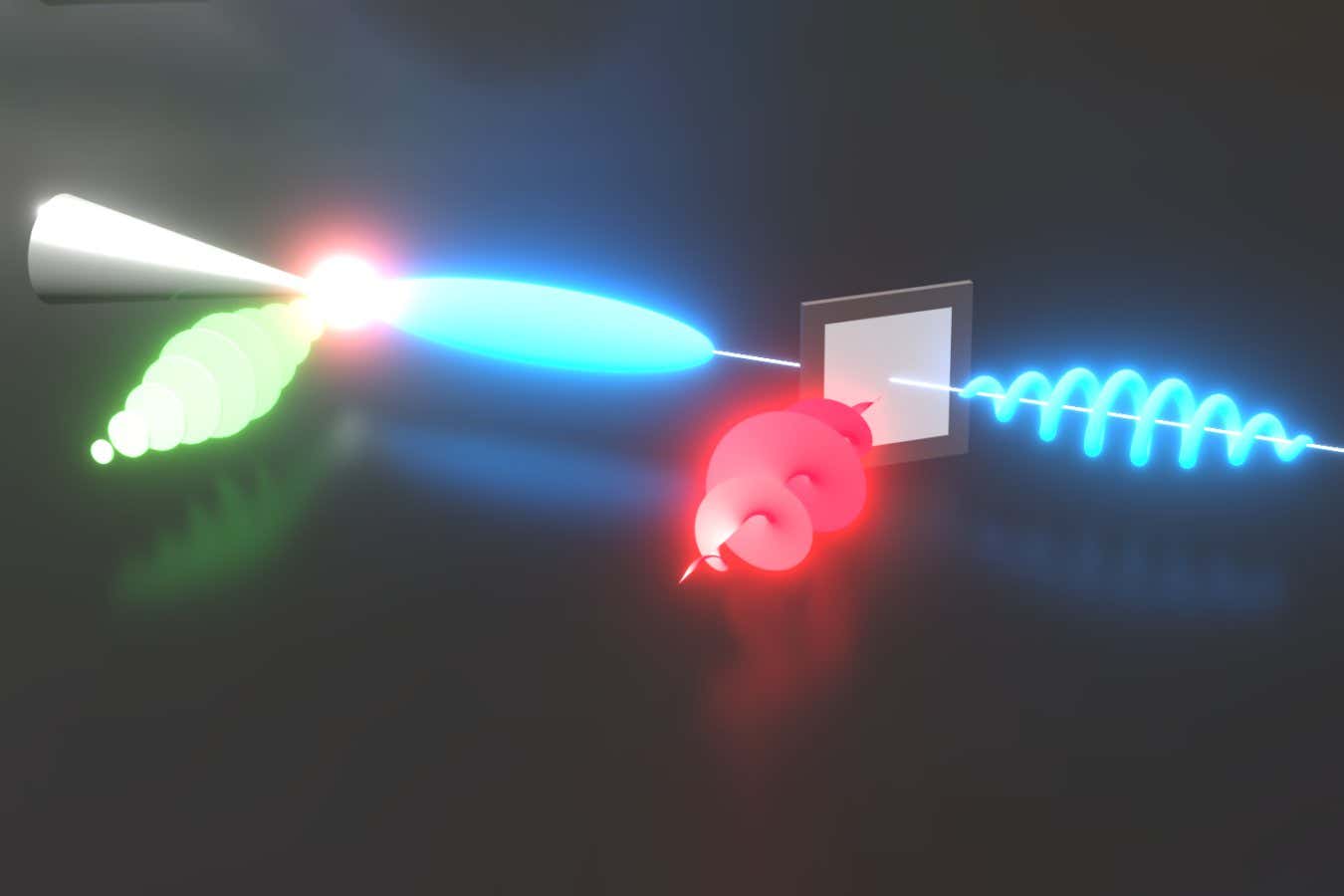
Science & Environment3 weeks agoLaser helps turn an electron into a coil of mass and charge
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoCaroline Ellison aims to duck prison sentence for role in FTX collapse
-
Business2 weeks ago
Eurosceptic Andrej Babiš eyes return to power in Czech Republic
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoNuclear fusion experiment overcomes two key operating hurdles
-
 Science & Environment3 weeks ago
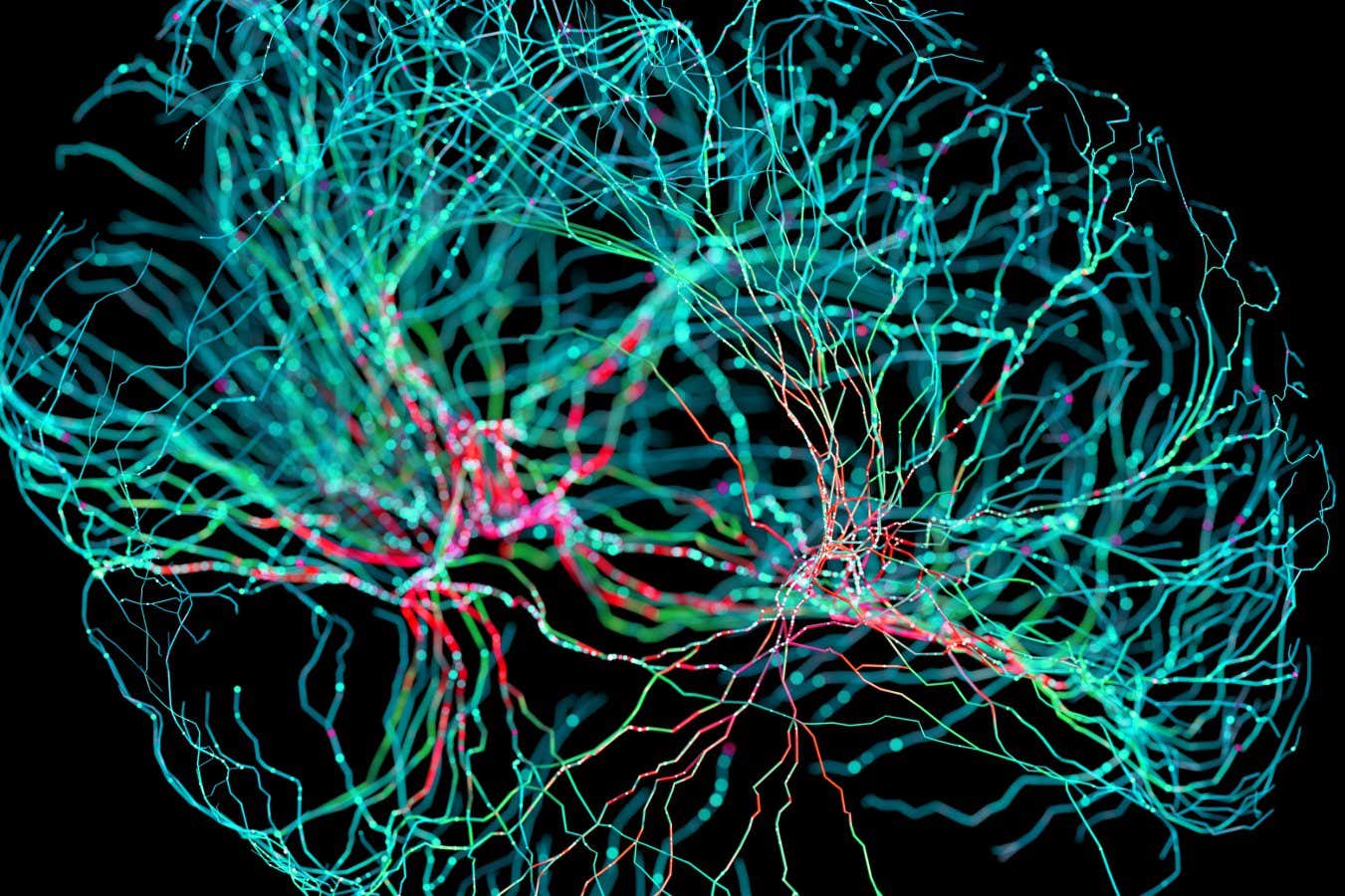
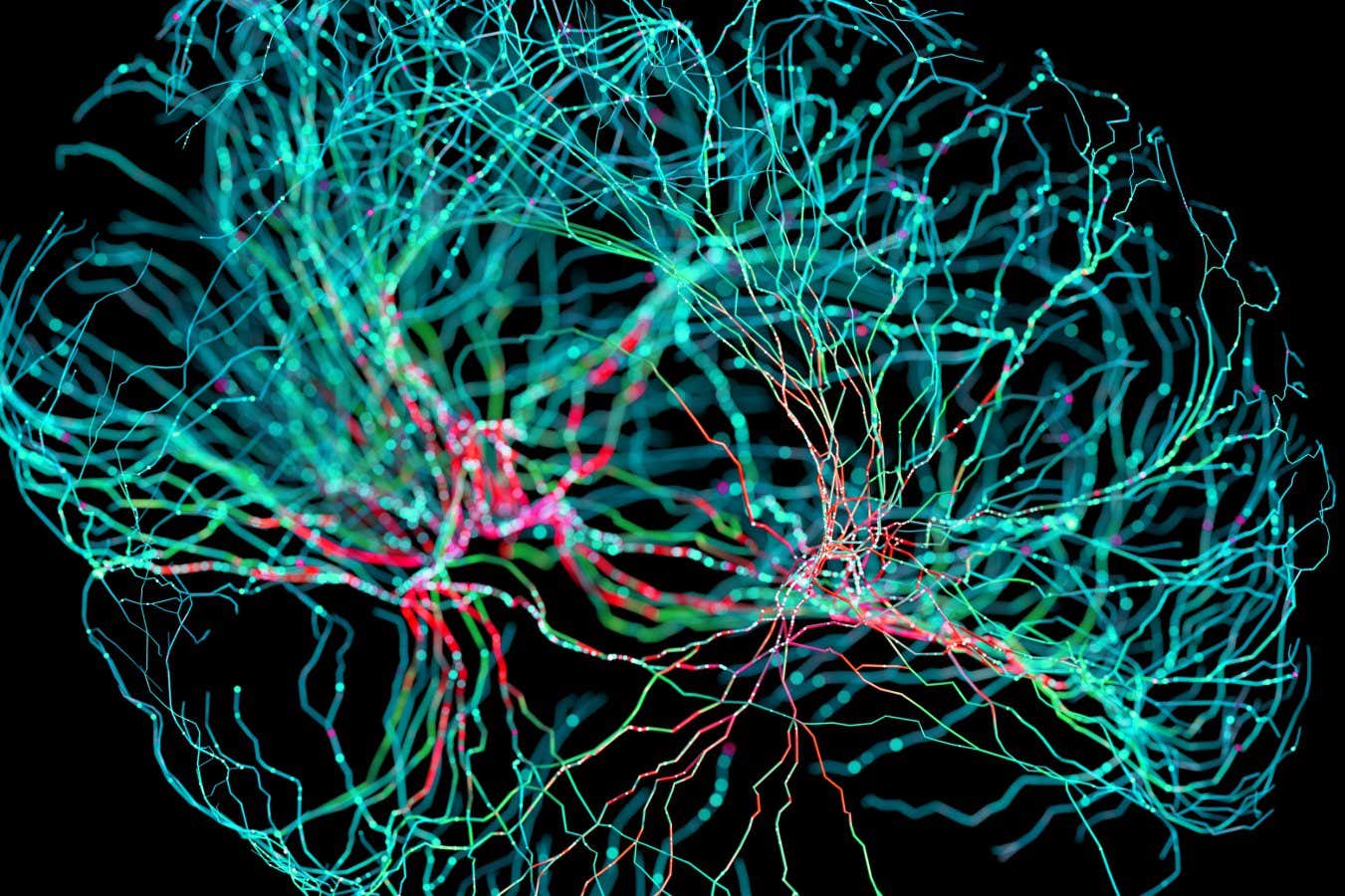
Science & Environment3 weeks agoNerve fibres in the brain could generate quantum entanglement
-
 Technology2 weeks ago
Technology2 weeks ago‘From a toaster to a server’: UK startup promises 5x ‘speed up without changing a line of code’ as it plans to take on Nvidia, AMD in the generative AI battlefield
-

 Football2 weeks ago
Football2 weeks agoFootball Focus: Martin Keown on Liverpool’s Alisson Becker
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoRethinking space and time could let us do away with dark matter
-

 News3 weeks ago
News3 weeks ago▶️ Hamas in the West Bank: Rising Support and Deadly Attacks You Might Not Know About
-
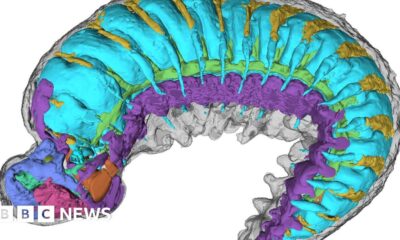
 Science & Environment2 weeks ago
Science & Environment2 weeks agoX-rays reveal half-billion-year-old insect ancestor
-

 MMA2 weeks ago
MMA2 weeks agoConor McGregor challenges ‘woeful’ Belal Muhammad, tells Ilia Topuria it’s ‘on sight’
-

 News3 weeks ago
News3 weeks ago▶️ Media Bias: How They Spin Attack on Hezbollah and Ignore the Reality
-
Business2 weeks ago
Should London’s tax exiles head for Spain, Italy . . . or Wales?
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoA new kind of experiment at the Large Hadron Collider could unravel quantum reality
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoA slight curve helps rocks make the biggest splash
-
 News3 weeks ago
News3 weeks agoNew investigation ordered into ‘doorstep murder’ of Alistair Wilson
-

 News3 weeks ago
News3 weeks agoIsrael strikes Lebanese targets as Hizbollah chief warns of ‘red lines’ crossed
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoFuture of fusion: How the UK’s JET reactor paved the way for ITER
-
 Technology2 weeks ago
Technology2 weeks agoQuantum computers may work better when they ignore causality
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoUK spurns European invitation to join ITER nuclear fusion project
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoWhy we need to invoke philosophy to judge bizarre concepts in science
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoCardano founder to meet Argentina president Javier Milei
-

 News2 weeks ago
News2 weeks agoWhy Is Everyone Excited About These Smart Insoles?
-

 Science & Environment2 weeks ago
Science & Environment2 weeks agoMeet the world's first female male model | 7.30
-
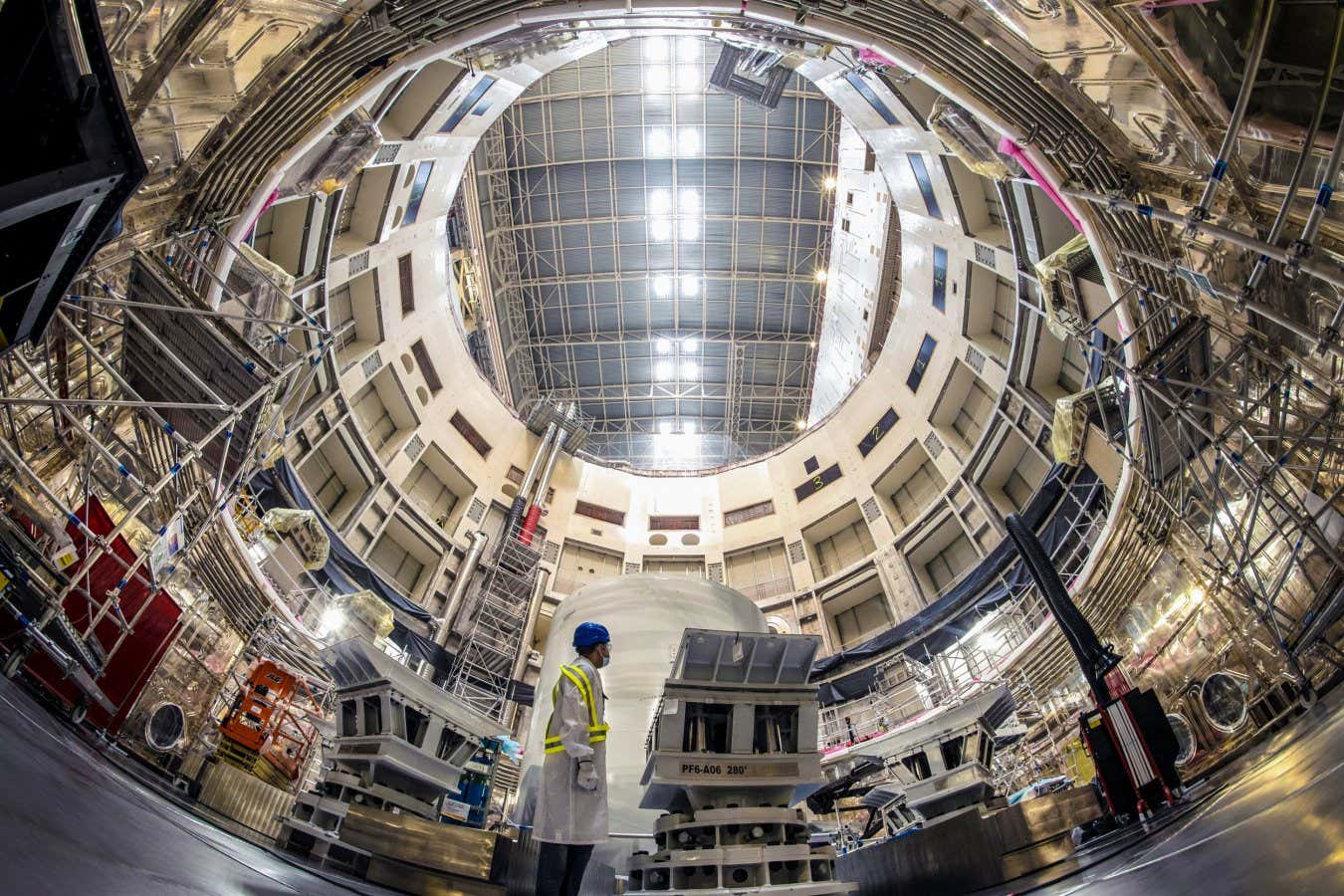
 Technology2 weeks ago
Technology2 weeks agoRobo-tuna reveals how foldable fins help the speedy fish manoeuvre
-

 Technology2 weeks ago
Technology2 weeks agoGet ready for Meta Connect
-

 Health & fitness2 weeks ago
Health & fitness2 weeks agoThe 7 lifestyle habits you can stop now for a slimmer face by next week
-

 Sport2 weeks ago
Sport2 weeks agoWatch UFC star deliver ‘one of the most brutal knockouts ever’ that left opponent laid spark out on the canvas
-
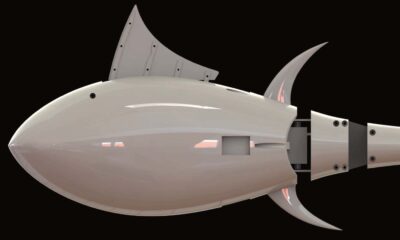
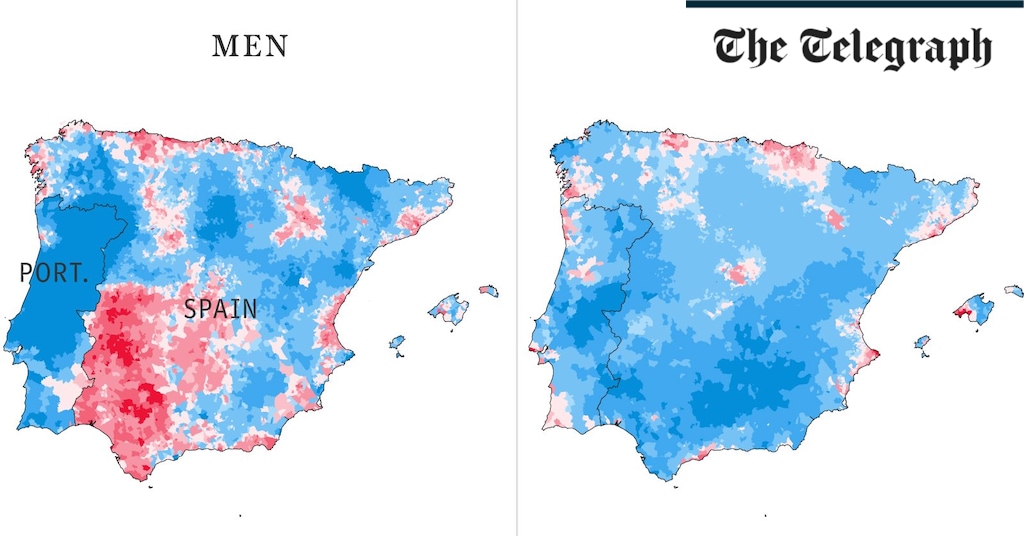 Health & fitness3 weeks ago
Health & fitness3 weeks agoThe maps that could hold the secret to curing cancer
-

 Technology3 weeks ago
Technology3 weeks agoThe ‘superfood’ taking over fields in northern India
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoA tale of two mysteries: ghostly neutrinos and the proton decay puzzle
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoLow users, sex predators kill Korean metaverses, 3AC sues Terra: Asia Express
-
News3 weeks ago
The Project Censored Newsletter – May 2024
-
Politics3 weeks ago
UK consumer confidence falls sharply amid fears of ‘painful’ budget | Economics
-

 Womens Workouts3 weeks ago
Womens Workouts3 weeks agoBest Exercises if You Want to Build a Great Physique
-

 Womens Workouts3 weeks ago
Womens Workouts3 weeks agoEverything a Beginner Needs to Know About Squatting
-

 News2 weeks ago
News2 weeks agoFour dead & 18 injured in horror mass shooting with victims ‘caught in crossfire’ as cops hunt multiple gunmen
-

 Womens Workouts2 weeks ago
Womens Workouts2 weeks ago3 Day Full Body Toning Workout for Women
-

 Sport3 weeks ago
Sport3 weeks agoUFC Edmonton fight card revealed, including Brandon Moreno vs. Amir Albazi headliner
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoEthereum is a 'contrarian bet' into 2025, says Bitwise exec
-

 Health & fitness3 weeks ago
Health & fitness3 weeks agoThe secret to a six pack – and how to keep your washboard abs in 2022
-
Business3 weeks ago
JPMorgan in talks to take over Apple credit card from Goldman Sachs
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoQuantum time travel: The experiment to ‘send a particle into the past’
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoBeing in two places at once could make a quantum battery charge faster
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoBitcoin miners steamrolled after electricity thefts, exchange ‘closure’ scam: Asia Express
-
 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoDorsey’s ‘marketplace of algorithms’ could fix social media… so why hasn’t it?
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoDZ Bank partners with Boerse Stuttgart for crypto trading
-
 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoBitcoin bulls target $64K BTC price hurdle as US stocks eye new record
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoBlockdaemon mulls 2026 IPO: Report
-

 TV2 weeks ago
TV2 weeks agoCNN TÜRK – 🔴 Canlı Yayın ᴴᴰ – Canlı TV izle
-

 Science & Environment2 weeks ago
Science & Environment2 weeks agoCNN TÜRK – 🔴 Canlı Yayın ᴴᴰ – Canlı TV izle
-

 Servers computers2 weeks ago
Servers computers2 weeks agoWhat are the benefits of Blade servers compared to rack servers?
-

 Technology2 weeks ago
Technology2 weeks agoIs sharing your smartphone PIN part of a healthy relationship?
-

 News2 weeks ago
News2 weeks agoUS Newspapers Diluting Democratic Discourse with Political Bias
-

 Technology2 weeks ago
Technology2 weeks agoThe best robot vacuum cleaners of 2024
-
Business1 week ago
Ukraine faces its darkest hour
-

 News3 weeks ago
News3 weeks agoChurch same-sex split affecting bishop appointments
-

 Politics3 weeks ago
Politics3 weeks agoTrump says he will meet with Indian Prime Minister Narendra Modi next week
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoHow one theory ties together everything we know about the universe
-

 News3 weeks ago
News3 weeks agoBrian Tyree Henry on voicing young Megatron, his love for villain roles
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoTiny magnet could help measure gravity on the quantum scale
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoHow do you recycle a nuclear fusion reactor? We’re about to find out
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoDecentraland X account hacked, phishing scam targets MANA airdrop
-
 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoRedStone integrates first oracle price feeds on TON blockchain
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks ago‘No matter how bad it gets, there’s a lot going on with NFTs’: 24 Hours of Art, NFT Creator
-
Business3 weeks ago
Thames Water seeks extension on debt terms to avoid renationalisation
-
Business3 weeks ago
How Labour donor’s largesse tarnished government’s squeaky clean image
-
Politics3 weeks ago
‘Appalling’ rows over Sue Gray must stop, senior ministers say | Sue Gray
-

 News3 weeks ago
News3 weeks agoBrian Tyree Henry on voicing young Megatron, his love for villain roles
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoCoinbase’s cbBTC surges to third-largest wrapped BTC token in just one week
-

 MMA3 weeks ago
MMA3 weeks agoRankings Show: Is Umar Nurmagomedov a lock to become UFC champion?
-

 Travel2 weeks ago
Travel2 weeks agoDelta signs codeshare agreement with SAS
-

 Politics2 weeks ago
Politics2 weeks agoHope, finally? Keir Starmer’s first conference in power – podcast | News
-

 Technology3 weeks ago
Technology3 weeks agoiPhone 15 Pro Max Camera Review: Depth and Reach
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoCrypto scammers orchestrate massive hack on X but barely made $8K
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoSEC asks court for four months to produce documents for Coinbase
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks ago‘Silly’ to shade Ethereum, the ‘Microsoft of blockchains’ — Bitwise exec
-

 Womens Workouts3 weeks ago
Womens Workouts3 weeks agoHow Heat Affects Your Body During Exercise
-

 Womens Workouts3 weeks ago
Womens Workouts3 weeks agoKeep Your Goals on Track This Season
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoPhysicists have worked out how to melt any material
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoSingle atoms captured morphing into quantum waves in startling image





You must be logged in to post a comment Login