Health & fitness
The 7 reasons your penis might be shrinking – and how you can stop it before it’s too late

PENISES come in all sorts of shapes and sizes and most men tend to be pretty well acquainted with how their member looks.
The appearance of your penis probably won’t change much throughout your life – though it might temporarily appear smaller when you’re chilly.
But sometimes penises do shrink for reasons that have nothing to do with the cold – and it may be permanent.
According to superintendent pharmacist at Chemist Click, Abbas Kanani, the shrinking and reduction of size in your penis is known as penile atrophy.
“If you’ve ever noticed your manhood appears smaller than usual, it can be hard to accept,” he says.
Penile atrophy can happen for a number of reasons, including medical conditions, hormonal imbalances, how much you exercise and the inevitable process of ageing.
Read more on sexual health
Here we go through seven key reasons why your penis may be looking smaller – and when you can do something about it.
1. You’re getting older
Your body goes through many changes as you naturally age, some of which impact sexual function.
Your penis is one body part that you might start to see change as the years go by.
“As men get older, blood flow reduces and penile tissues receive less oxygen and essential nutrients,” Abbas explains.
“When this happens over a prolonged period of time, it can lead to tissue damage and atrophy.
“Blood flow issues also cause the tissues to lose elasticity, making it more challenging to stretch and maintain your penis’ normal length and girth size.”
Another side effect of reduced blood flow could be an “increase in collagen, which can lead to fibrosis, the thickening and scarring of tissue”, the pharmacist adds.
“This can reduce the overall size and elasticity of your penis.”
2. Your hormones are imbalanced
Hormones can also affect the look of your penis.
Testosterone is a crucial hormone for male sexual health, which tends to decline as you age.
According to Abbas: “Testosterone preserves your penis’ structure, the function of smooth muscle and connective tissue.
“When these are no longer being maintained because of a decline in hormones, shrinkage can happen over time.”
Aside from a difference in size, you may also notice your erections becoming less frequent or weaker as testosterone levels wane.
“This means that your penis is no longer benefiting from the stretching effect that helps to maintain its size and elasticity, which can lead to a gradual decrease in penile size,” Abbas says.
While ageing is a common cause, it could be down to other imbalances.
3. You’re a smoker
Smoking can decimate your body in a number of ways and your penis is yet another part that can suffer.
“There are chemicals found in cigarettes, such as nicotine and carbon monoxide, which cause blood vessels to constrict and reduce blood flow,” Abbas notes.
“They also decrease the production and availability of nitric oxide, which is vital for the dilation of blood vessels and the initiation of erection.”
Yep, you heard right – smoking can also affect your ability to hold and maintain an erection, as it increases your risk of erectile dysfunction.
According to Abbas, it can mean your penis is not stretched and oxygenated on a regular basis, which can lead to overall shrinkage.
Penis fact vs. fiction
Though penises are the subject of much contemplation, certain myths around them reign rampant – from shoe size reflecting the size of your member, to creams and oils being able to make it larger.
On top of this, it can often feel taboo or embarrassing to ask questions about your private parts.
GP and author Dr Philippa Kaye answers burning questions you might have about your nether regions.
What is the average penis size?
The average size of a penis is approximately 9cm when flaccid/soft and about 13cm when erect.
Does your shoe size reflect your penis size?
No.
A study looking at the penises of over 100 men of varying ages looked at shoe size and penis length and found no correlation between the two.
Why is the penis shaped like a mushroom?
So, there is a ridge between the top of the shaft of the penis and the glans, which is shaped rather like a mushroom.
One theory as to why this is is known as the ‘semen displacement theory’, which suggests that the shape of this ridge essentially scoops out and removes any sperm left behind in the vagina by a previous partner, who might be a genetic rival evolution-wise.
Can you break your penis?
There are no bones in the penis, but you can still break it.
During an erection there are spongy tissues called corpus cavernosum, which fill with blood to make the penis erect.
If there is a trauma, often a violent twisting or bending motion when the penis is erect, then part of the covering of the corpus cavernosum called the tunica albuginea can burst, leading to bleeding into the penis and a very painful swelling.
It is rare and tends to occur during sex, often when a partner is on top.
Read more on penis facts and fiction here.
4. You have Peyronie’s disease
Peyronie’s disease is a condition that causes your penis to curve when it’s erect.
It typically affects men over 40, but younger men can also get it.
Abbas explains: “Fibrous plaques form within the penis and this can prevent the penis from expanding evenly, causing it to painfully bend, during an erection.
“If this happens over time, the penis can shorten typically where the plaque is situated on the penis.”
The condition can lead to a loss of elasticity in the penis when it’s both erect and flaccid, which can make shrinkage of your member worse.
According to the NHS, symptoms of Peyronie’s disease include:
- Swelling that later causes a hard lump to develop on the shaft of your penis and stops it stretching during erections
- A curve in your penis when it’s erect (if the hard area is on the top of your penis it will curve upwards, if it’s on the bottom it will curve downwards)
- Painful erections that can make having sex difficult
- Problems getting or keeping an erection (erectile dysfunction)
- Other changes to your penis – for example, you may have a hard area on the top, bottom and side of your penis, shortening it and making it narrower in the middle
If you have Peyronie’s disease, your skin may also be thicker and less flexible in other parts of your body, such as in your hands and feet.
5. You’re taking certain medications
If you’ve been prescribed medications, it’s important to continue taking them.
But some can take an effect on the size of your penis over time, Abbas says.
“Regular erections are important for the health of your penis because they increase blood flow and oxygenation of the tissues,” the pharmacist explains.
“Some medications, such as hormonal and hair loss treatments, antidepressants and high blood tablets can impede on hormonal balance, blood flow and nerve function, contributing to penile atrophy.
“Some drugs also suppress the production or reduce the conversion of testosterone and impact blood flow to the penile tissue.”
6. You have chronic diseases
Whether you have diabetes, cardiovascular disease or cancer, these chronic conditions may make a mark on your penis.
For diabetes sufferers, blood flow can be an issue.
“Blood vessel damage caused by high blood sugar levels in people with diabetes impair the supply of blood to the penis,” Abbas says.
“As a result, tissues can become deprived of oxygen and nutrients causing shrinkage.
“Cardiovascular disease causes plaque to build up in the arteries and restricts blood flow around the body, including the penis causing it to appear shorter in length.
“In chronic cases, atrophy can become permanent”.
Both diabetes and cardiovascular disease can increase your risk of experiencing erection issues.
Men with prostate cancer may also notice a change in penis size, as radiation therapy has been linked to shrinkage.
A small study found that patients undergoing prostate cancer treatment saw a gradual decrease in the length of their penis when stretched.
7. You’re overweight or not exercising enough
Finally, your weight and levels of exercise can both affect your todger.
“Poor circulation and hormonal imbalances can occur if you do not exercise enough or are overweight,” Abbas says.
“Not only is this bad for your overall health and well-being, it can also directly affect your ability to get or maintain an erection and your body’s ability to produce enough sex hormones.
“Physical activity helps to boost circulation and maintain healthy testosterone levels.”
Should I worry about penis shrinkage?
Though it can be concerning to see your member shrink before your eyes, Abbas says it can be managed with the right approach.
“One of the most noticeable signs and symptoms is a reduction in length and girth, but you may also notice a loss of elasticity leaving your penis feeling stiff even when not erect,” he says.
“You may also have weaker erections, decreased sensations when stimulated or changes in appearance of your penis such as wrinkling, curving or indentation.
“Men should book an appointment with their GP if they think they may be experiencing penile atrophy, so you can be correctly diagnosed and offered the most appropriate treatment.”
To help avoid shrinkage, you could also take steps to address any of the concerns above, such as quitting smoking, getting active and speaking to a doctor about any medications you are taking.
Womens Workouts
Day 17 – 30 MIN FULL BODY BURNER HIIT WORKOUT – Full Body, No Equipment, No Repeat

We’re on a roll team! It’s Day 17 of the GROW Challenge and we’ve got another Super Sweaty HIIT Workout to crush together! 30 minutes of full-body, high intensity, fat-burning exercises. Let’s get our heart rate up, push yourself a little extra today – I promise you’ll feel AMAZING! Let’s do it!!
WORKOUT DETAILS
👉🏼 Duration: 30 MINS (Plus 5 mins of cool-down stretches)
👉🏼 Intensity: Super Sweaty 💧💧💧
👉🏼 No Equipment
👉🏼 50 Sec Work, 10 Sec Rest
👉🏼 No Repeat
Please remember that we are all different and that you can make this your OWN workout… take a longer break when you need to.
Music: https://www.epidemicsound.com
📷 GEAR I USE:
Camera: https://amzn.to/3aticKD
Lens: https://amzn.to/3cCiujR
Tripod: https://amzn.to/2zontX9
Microphone: https://amzn.to/34VaKXH
💪🏼 MY HOME TRAINING GUIDE: http://growingannanas.com
» Subscribe to my Channel for weekly workouts: http://bit.ly/2QLvpXn
» Instagram: http://bit.ly/2ZSdHFR
» Facebook: http://bit.ly/2SVkgpE
✉ Contact (business inquiries): anna@fyndafit.com
D I S C L A I M E R
If you are a newbie start with a simple and easy exercise before attempting all advanced exercises. Performing exercises out of your capability might strain your muscles and you may get injured.
This channel offers health, fitness and nutritional information. You should not rely on this information as a substitute for, nor does it replace, professional medical advice, diagnosis, or treatment. By performing any fitness exercises without supervision like with this video, you are performing them at your own risk. See a fitness professional to give you advice on your exercise form. Growingannanas will not be responsible or liable for any injury or harm you sustain as a result of this video.
source
Health & fitness
Urgent call to shut down ‘rogue BBL clinics’ after mum, 33, becomes first in UK to die from dodgy op

SHUT down rogue butt-lift clinics and only let qualified doctors do them, top surgeons have warned.
The Joint Council of Cosmetic Practitioners issued the plea on Thursday after a 33-year-old Brit mum died in September following a botched BBL.
Brazilian butt-lifts, also known as buttock augmentation procedures, involve injecting fat or filler into the bum to shape it.
But wrongly injecting too deep into the buttock can pump chemicals into the bloodstream and cause deadly clots, infections or sepsis.
They can also go wrong if the anaesthetic is bungled or people have allergies.
Two people were arrested on suspicion of manslaughter after mum-of-five Alice Webb, from Gloucestershire, died in September following complications of the procedure.
She became the first person to die this way in Britain, although others have suffered fatal ordeals after surgery abroad.
UK regulation is lax as they can be considered “non-surgical” and untrained beauticians can get the kit to do them.
A lack of regulation for unlicensed medical practitioners puts people’s health at serious risk, particularly with buttock fillers
Elaine Sassoon
The JCCP said BBLs must be classified as surgical procedures and strictly controlled so that only qualified, registered and experienced plastic surgeons can do them.
The British Association of Aesthetic Plastic Surgeons, which only recently ended a four-year plea for members not to do the procedure at all, co-signed the report.
The Sun has called on ministers to tighten regulation of fillers and cosmetic procedures in our Had Our Fill campaign.
Elaine Sassoon, a member of the BAAPS council, said: “The cosmetic sector faces a lack of regulation for unlicensed medical practitioners.
“This puts people’s health at serious risk, particularly with buttock fillers for BBL.
“While specialist surgeons follow safety guidelines, untrained individuals can inject unsafe, bulk-purchased products in unregulated settings.”
The report said the same rules should be applied to any procedures on the genitals or breasts.
It said: “These procedures should only be performed by appropriately trained specialist plastic surgeons and fully qualified General Medical Council registered medical doctors who possess additional qualifications and have proven competence.”
Tragic mum told she didn’t need work done
Alice Webb, herself an aesthetic practitioner, had travelled to a training session where she would learn how to perform the procedure before having her own done.
But cops rushed to a house at around 11.30pm that night after the alarm was raised, with ambulances already at the scene.
Alice was taken to Gloucestershire Royal Infirmary but died in the early hours of Tuesday, September 24.
The tragedy happened after her cousin, Dianna Webb, told her she did not need the procedure.
A tearful Dianna, who calls herself Alice’s “second mum” as she helped raise her, told The Sun: “We had talked about it a lot before she went to have the procedure.
“She had told me she was going to have this done and I said she didn’t need it – she already looked beautiful.
“And she was stunning on her own.
“We were on the phone for two hours before she went. Alice said they seemed really professional and put her at ease about the procedure.
“She was not one of these people that would go and just have something done without looking at every little detail first, obviously because she worked in the industry too.
“Alice put her heart into her work.
“She took every course she could take, including this one, because she wanted to make sure she got everything right.”
Dianna said her family would demand the government ban liquid BBL injections to make sure Alice’s death was “the first and the last” on British shores.
A Department of Health spokesperson said: “Our deepest sympathies are with Alice’s family and friends in this tragic case, which is incredibly concerning.
“The safety of patients is paramount, and we would urge anyone considering a cosmetic procedure to consider the possible health impacts and find a reputable, insured, and qualified practitioner.
“Work is ongoing to explore options around oversight of the non-surgical cosmetics sector and we will provide an update at the earliest opportunity.”
What are Brazilian Bum Lifts and why are they so popular?
Buttock enlargement surgery – known as a Brazilian bum-lift (BBL) – is used to make the bum look bigger, rounded and lifted.
Surgeons transfer fat, inject filler or insert silicone-filled implants.
It is the fastest growing cosmetic procedure but also one of the most dangerous, according to the British Association of Aesthetic Plastic Surgeons (BAAPS).
Many patients are travelling to the likes of Turkey or seeking out unregistered surgeons in the UK and are not given full information on the risks.
BBLs carry the highest risk of all cosmetic surgeries – with more than one death occurring per 4,000 procedures.
Due to celebrities undergoing such ops, many women are hoping to emulate their looks.
Consultant clinical psychologist Dr Anu Sayal-Bennett, a chartered member of the British Psychological Society, told the BBC: “Despite there being so much about body positivity, there are pressures for women – and men too – to look a certain way.”
Many people travel abroad for the procedure because it is cheaper and advertising is “terribly seductive”, combined with the idea of a beach holiday, added Dr Sayal-Bennett.
Health & fitness
Mum-of-two, 32, with ‘vampire disease’ vomits 30 times a day and lives in fear of dropping dead at dinner

A MUM-of-two says she lives in fear of dropping dead at the dinner table due to a condition known as “vampire disease”.
The rare disorder, known as acute intermittent porphyria, means Phoenix Nightingale has to avoid garlic at all costs.
The 32-year-old could have a potentially “fatal attack” if she eats too much of the allium, which contains sulphur.
During an attack, she can suffer severe pain, migraines and constipation for three days at a time.
Eating garlic could also leave her vomiting up to 30 times a day, Phoenix said.
Her immune system crashes during an attack, causing her body to go into shock, meaning she could stop breathing.
Read more on rare diseases
As a result, eating sulphur-rich garlic could be fatal.
Porphyrias are a group of uncommon disorders caused by problems with the production of chemicals called porphyrins in the body, according to the NHS.
Porphyrins are the chemical building blocks of haem, which form haemoglobin, the component of red blood cells that allows oxygen to be carried around the body.
There are eight different types of porphyria disorders, which affect the skin and nervous system.
If the disorder is ‘acute’ – as in Phoenix’s case – the onset of symptoms can be rapid.
They can include stomach pain, nausea and vomiting, changes in blood pressure or increased heart rate, muscle weakness, paralysis, anxiety, confusion, hallucinations and seizures.
It’s believed that vampire myths – such as that of Count Dracula – sprung out of porphyria.
According to Michael Hefferon, assistant professor at the Department of Paediatrics at Queen’s University, some patients with porphyria suffer with sensitivity to light, receding gums that make teeth look like fangs, dark red urine – which led people of yore to think they were drinking blood – and aversion to garlic due to attacks.
“People call it the vampire disease,” Phoenix, of Robbinsdale, near Minneapolis, Minnesota, US, said.
“Count Dracula had it. It comes from the legend about them needing to avoid garlic, having to stay out of the sun, looking pale and having receding teeth.
“Neurological side effects can make people think that those with the condition must have been monsters or are possessed.”
The mum was first diagnosed with acute intermittent porphyria in August 2023.
“There’s too much sulphur in garlic and I have a sulphur allergy,” she said.
“I avoid sulphurs in general. Eating garlic in high amounts or over an extended period could be fatal.
“I haven’t eaten garlic since I was diagnosed. I could never eat garlic bread. It could send me into an attack.
“Attacks happen when the body reaches a toxic load large enough to make it crash.
“It’s life-threatening for me. When I have an attack, my body wants to exit everything.
“I’ll puke 60 times over two days. I can stop breathing and it can cause paralysis.
“I’ve almost died. Different foods and things I ingest can make me have an attack.
“Sometimes there can be a buildup, so if I have small amounts of a certain food over a few days.
“Symptoms can start one to two weeks before an attack or it can come out of nowhere.”
What is acute intermittent porphyria?
Porphyria is the name given to a group of very rare metabolic disorders that occur when your body is unable to produce enough of a substance called haem.
Haem is required for many bodily functions.
It is a component of haemoglobin, a vital protein which helps transport oxygen around your body and the pigment that gives red blood cells their colour.
Acute porphyrias are characterised by attacks of pain and other signs of neurological distress.
The majority of people who inherit the disorder do not have attacks.
Where symptoms do occur, they are sudden and can last for days or weeks.
They can include:
- Anxiety, restlessness and insomnia
- Severe abdominal pain
- Pain in your arms, legs or back
- Vomiting and constipation
- High blood pressure (hypertension)
- Muscle pain, tingling, numbness, weakness or paralysis
- Confusion, hallucinations and seizures
- Breathing difficulties (respiratory paralysis), possibly requiring ventilation
- Reddish coloured urine
Acute attacks happen when the levels of porphyrins in your body become very elevated.
They range in severity and usually require having to go to hospital. In the worst case they may require emergency procedures to prevent death.
Source: British Liver Trust
The mum-of-two says she’s suffered with symptoms since she was a baby but struggled to get a diagnosis as the condition is so rare.
She has had more than 480 attacks in her life and says that they’re “more painful than childbirth”.
Phoenix said: “I had one attack where I didn’t go to hospital and it went on for 40 hours. It was non-stop vomiting, losing consciousness, screaming and crying.
“It was horrific pain that prescription pain medication hardly touches.
“I’ve pushed out two children and it’s worse than childbirth. It’s agony.”
DINNER DRAMA
Phoenix says going out for dinner is upsetting as she worries about what ingredients will be in her meal.
She said: “When I go out for dinner, unless it’s a place I know, I look at a menu and I cry because I don’t know what I can eat and prefer to stick with my safe foods.
“I can’t eat red grapes, coffee or soy and I can’t have any alcohol at all.”
She is sharing her story to help raise awareness of the condition, as it took Phoenix 31 years to get a diagnosis.
Phoenix said: “It’s hard as a diagnosed person not being able to find a doctor who can help. When I see a doctor or go to hospital, they have to google the condition.
“It took 31 years to get diagnosed and I had to pay out of pocket and spend years running analytics on it.
“I had to take it into my own hands.
“I’m very careful about what I put in my body. I avoid a lot of food. I stick to the food that I know is safe. I can’t even take most medications.
“It’s been a huge struggle for me.
“I have been through so much with my health so I’m very passionate about getting my health stable enough that I can someday help make changes in the medical system for mystery diagnoses and chronically ill patients.
“There has to be more people out there suffering with it and being called crazy.”
Womens Workouts
Mommy Belly Fat Lose Workout For Women #shorts #viral #fitness
Health & fitness
Girl, 19, died after GP prescribed ‘too many painkillers’ that triggered severe brain damage and stopped her heart

A TEENAGER who died after taking too many painkillers had been prescribed the pills despite two recent overdoses on the same medication, an inquest has heard.
Ellie Knight, 19, was given a month’s supply of the anti-inflammatory drug to manage back pain by a GP who later conceded with hindsight that he “should have given her less”.
The animal lover overdosed on the pills a fortnight after receiving her prescription and suffered a cardiac arrest – when the heart stops beating – and severe brain damage.
She was rushed to Queen Elizabeth The Queen Mother Hospital in Margate, Kent, but tragically died three weeks later on January 9.
Her family have now questioned why she was given such a large supply of the pills within two months of three previous overdoses – two of them involving the same drug.
An inquest into her death was told that Ellie had gone to Newington Road practice in Ramsgate on December 4 last year complaining of back pain.
GP Dr Geoffrey Kimanje believed seizures suffered in a separate overdose just a week earlier had led to inflammation in her joints, and there were suspicions she had hypermobility issues.
The hearing was told Ellie’s mother, Sarah Knight, was said to have been “angry about the doctor prescribing” a month’s worth of the medication as she had reportedly requested her daughter not be given the drug.
However, Dr Kimanje told the coroner he had been left with a difficult decision and had spoken to Mrs Knight – who did not attend the inquest – before issuing the prescription.
The GP said he did not recall any opposition, adding that he even made an agreement with Ellie and Mrs Knight that the teenager’s medication would be administered by her mother.
He told the hearing: “I thought this drug was the best option for anti-inflammatory [issues].
“I thought I’d get her something more restrictive in terms of it needing a prescription.
“I think it’s easy to say she should have had less tablets, but I didn’t want to be obstructive in her care.
“I took confidence in [the family]; in hindsight, I should have given her less.”
Despite the reported agreement, it was not made clear how or why Ellie had come to administer the drugs herself, though there was no suggestion her family were at fault.
When asked if there was anything he felt he should or could have done differently given the circumstances at the time, the GP said: “I don’t think so.”
The inquest heard Ellie had admitted to having thoughts of suicide since the age of 11 and had been under the care of mental health services.
Her family expressed concern that a reported promise of home visits they thought would be daily did not materialise, with Ellie visited just once by mental health teams.
But Kirsty Wade, an operational manager at the Kent and Medway NHS and Social Care Partnership Trust (KMPT), said no such offer should have been made and would not even have been possible in Ellie’s case, due to her often spiralling at night when home visits do not take place.
It was explained that Ellie did not engage particularly well with other mental health teams and the view at the time was that daily visits could have actually increased the risk of Ellie acting on the commands of “derogatory voices” in her head.
It was a cry for help, but we can’t change anything now
Sarah Knight
Mrs Wade said: “It was quite a complex picture.
“She’d been staying up late at night and had a poor structure but there was evidence of futuristic thinking and planning.
“She was also reluctant to utilise service contact numbers for support, as she didn’t like burdening other people with her problems.
“The risks were low enough that we could have managed them in the community, but she still potentially could have needed some extra support.
“She didn’t seem to have any coping strategies for when she was stressed.”
As well as the expected home visits falling through, it was explained that a psychiatric appointment had to be cancelled due to Ellie being in hospital following one of her overdoses. She died before it could be rearranged.
Coroner Catherine Wood said Ellie had sought help following her three previous overdoses.
She said at the time of the fourth, on December 18, it was not clear what Ellie’s intentions were.
‘NO EVIDENCE SHE WANTED TO DIE’
Delivering a narrative conclusion at the hearing in Maidstone on Friday, she expressed her condolences to Ellie’s family and explained why she could not rule her death a suicide.
“She was referred for a programme of psychological treatment which she sadly didn’t receive because of her death,” said Mrs Wood.
“I cannot say whether her being on that pathway would have changed the eventual outcome.
“We don’t have any evidence to suggest she wanted to die. I don’t have evidence she didn’t intend to die.
“We don’t know the facts – we weren’t there.
“[Dr Kimanje] gave the reasons for his prescription. I accept his evidence on this point. He also rang Ellie’s mother at the time of the consultation.
“Whilst I accept the evidence that we did hear, it may have been better to have a plan in relation to medication in the risk assessment process as part of a risk assessment at the mental health services.
“As coroners we see too many deaths of young people who die as a consequence of their own actions.
“It’s something that in this world we do see more than any of us would like to, but it’s very difficult for staff in a mental health setting to assess the risks here as to what can be done.
“I’d note that there is work to be done in terms of risk assessment and work has been undertaken and there have been reorganisations of services.”
She had such a big heart, and was loved by so many people – more than she knew
Sarah Knight
Mrs Wood added she would not be making a Prevention of Future Deaths Report, with mental health teams already undergoing changes in staff training and guidelines in response to recent events.
Ellie’s parents believe she did not intend to take her own life and previously said they wished she had accepted just how loved she was by everyone.
They said: “We don’t think she did it to end her life, or to get to the point it got to. It was a cry for help, but we can’t change anything.
“She had such a big heart, and was loved by so many people – more than she knew. We told her lots but she just didn’t accept it.
“Ellie did suffer from depression, she did have worries, and it played a big part in what happened.”
Born on June 14, 2004, Ellie was the middle child of three siblings, with 22-year-old Liam and five-year-old Robin completing the household.
The former Broadstairs and Canterbury College pupil aspired to work in animal or childcare, having a fondness for both, and studied health and social care.
A keen music lover with a wide range of tastes, she was also an avid watcher of TV, with Friends and Victorious among her favourite shows.
As an adult, Ellie developed an interest in motorbikes and had planned to buy one to do up with her dad, Michael.
Health & fitness
Exact number of days a month Brits feel their best revealed – as sore throats & lack of sleep hit

Brits only feel at their very best for 13 days a month, according to research.
A poll of 2,000 adults revealed they feel in good health for less than half the time (42 per cent) – the equivalent of only 152 days a year.
The rest of the time is spent with various ailments including colds, poor sleep, stress and digestive issues.
During the winter months, 31 per cent constantly feel run down with sniffles, coughs and sore throats.
And 40 per cent feel the effects of hayfever starting as early as April.
It also emerged 31 per cent were unaware of the link between good gut health and their immune system.
Gut microbiologist Dr Kate Steed from Optibac Probiotics, the friendly bacteria brand which commissioned the study, said: “It is extremely hard to feel 100 per cent at all times with so many bugs going round.
“Colds, cough and contagious bugs can hit at any time but are rife during the winter months, and then in the spring and summer hayfever comes along.
“Then there’s a whole range of digestive ailments that aren’t seasonal, like upset stomachs, bloating or trapped wind that can crop up regularly and often when you would least like them to.”
With so many health complaints, it’s no surprise 72 per cent are interested in boosting their immune system, so they can live life to the fullest (60 per cent), to be in good health for the family (44 per cent) and because they have simply had enough of catching coughs and colds (26 per cent).
The research found 69 per cent struggle with gastric issues, such as constipation (22 per cent), acid reflux (22 per cent) and stomach ache (22 per cent).
And 39 per cent of those deal with these symptoms as often as once a week.
But 76 per cent claim people who don’t have digestive issues don’t know how debilitating they can be, according to the OnePoll stats.
Dr Kate Steed added: “Digestive issues can really reduce quality of life, impacting social activities, relationships and even productivity at work.
“Having one less thing to worry about can be life changing.
“Studies indicate that maintaining a healthy gut plays a key role in overall wellness.
“Probiotics, known to benefit gut health, can be particularly effective when they contain carefully researched strains of beneficial bacteria.
“Those looking to try them should opt for strains backed by scientific evidence.”
-
 Science & Environment3 weeks ago
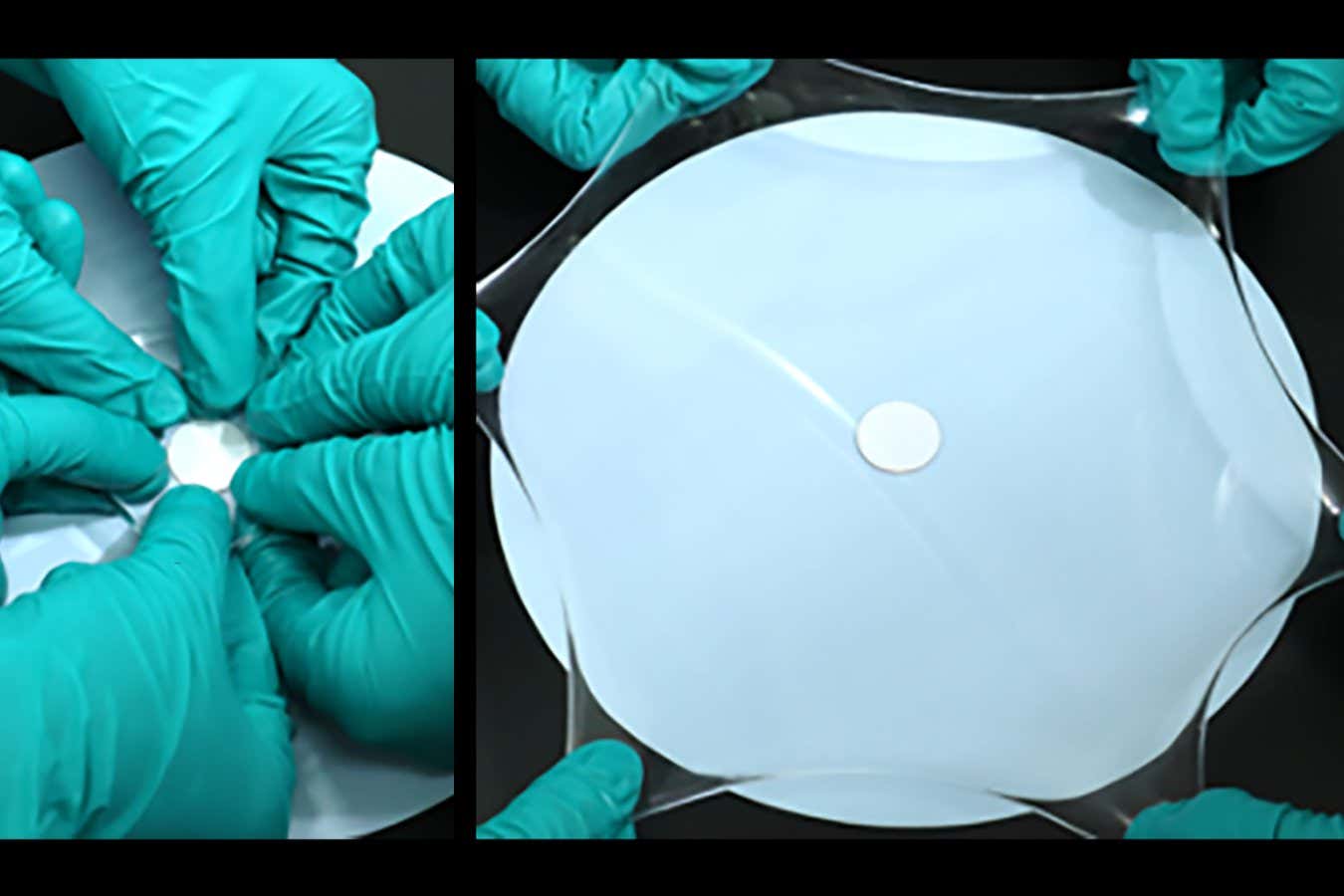
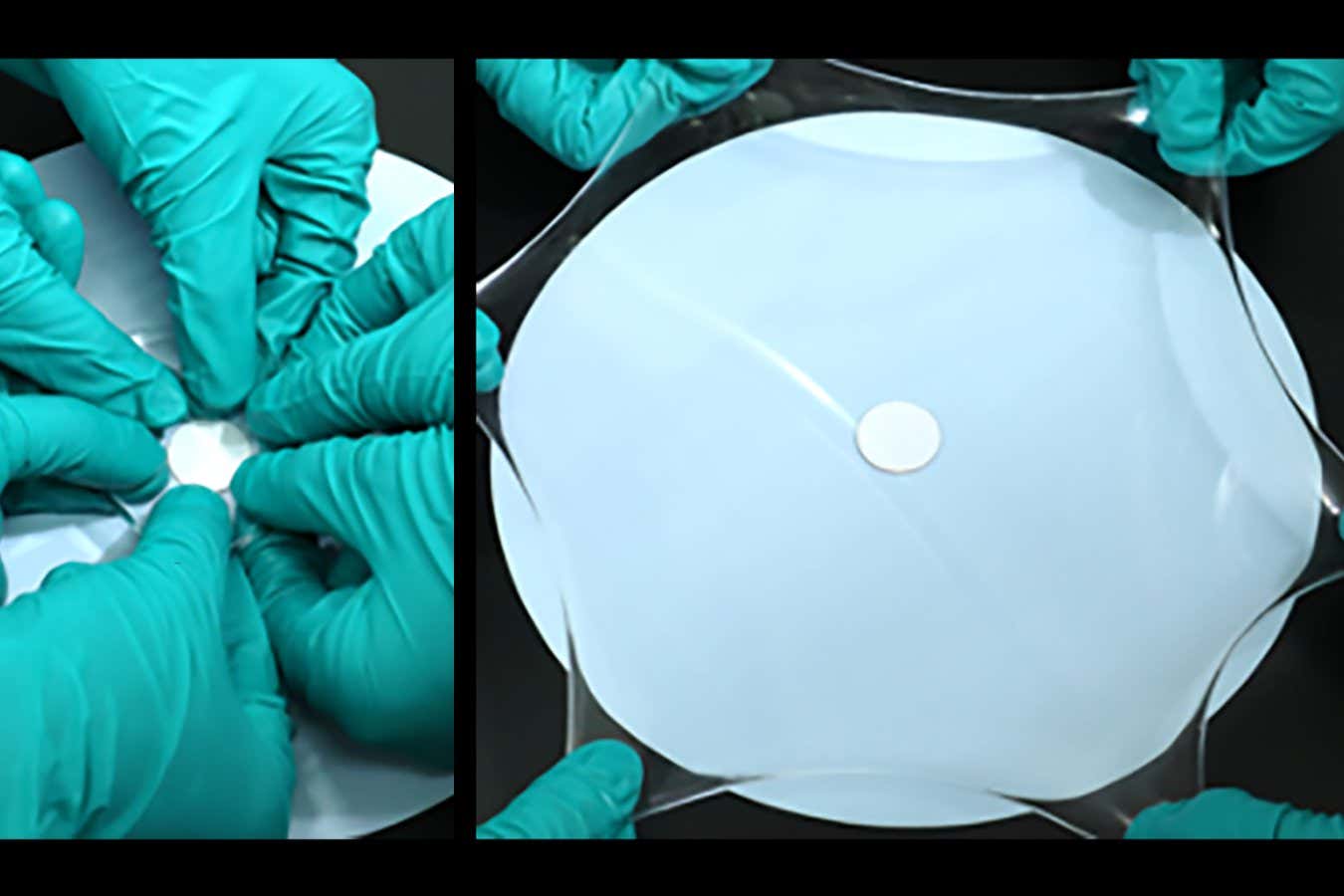
Science & Environment3 weeks agoHyperelastic gel is one of the stretchiest materials known to science
-
 Science & Environment3 weeks ago
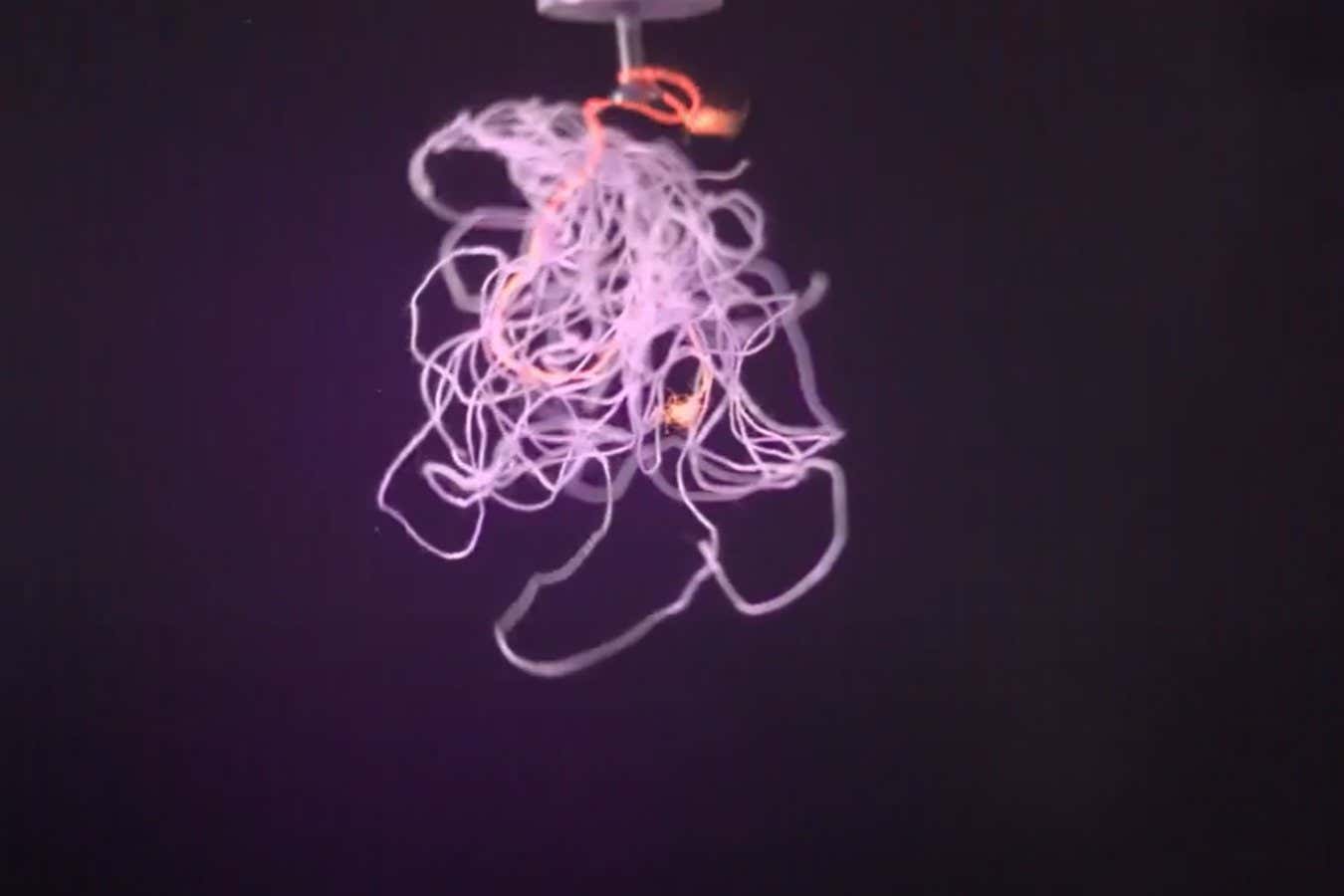
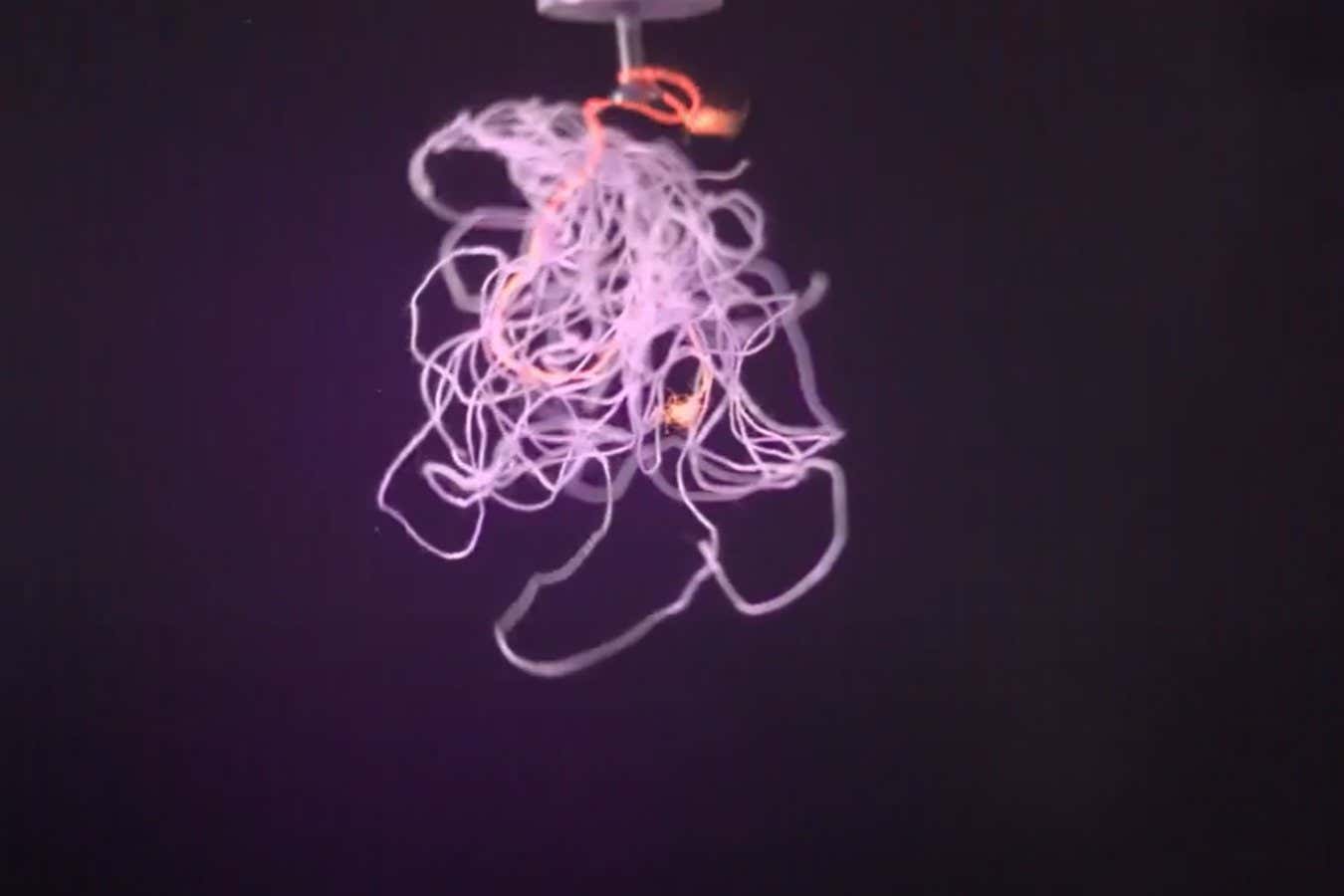
Science & Environment3 weeks agoHow to unsnarl a tangle of threads, according to physics
-

 Womens Workouts2 weeks ago
Womens Workouts2 weeks ago3 Day Full Body Women’s Dumbbell Only Workout
-

 Technology3 weeks ago
Technology3 weeks agoWould-be reality TV contestants ‘not looking real’
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoMaxwell’s demon charges quantum batteries inside of a quantum computer
-

 Science & Environment3 weeks ago
Science & Environment3 weeks ago‘Running of the bulls’ festival crowds move like charged particles
-
News3 weeks ago
the pick of new debut fiction
-

 Science & Environment3 weeks ago
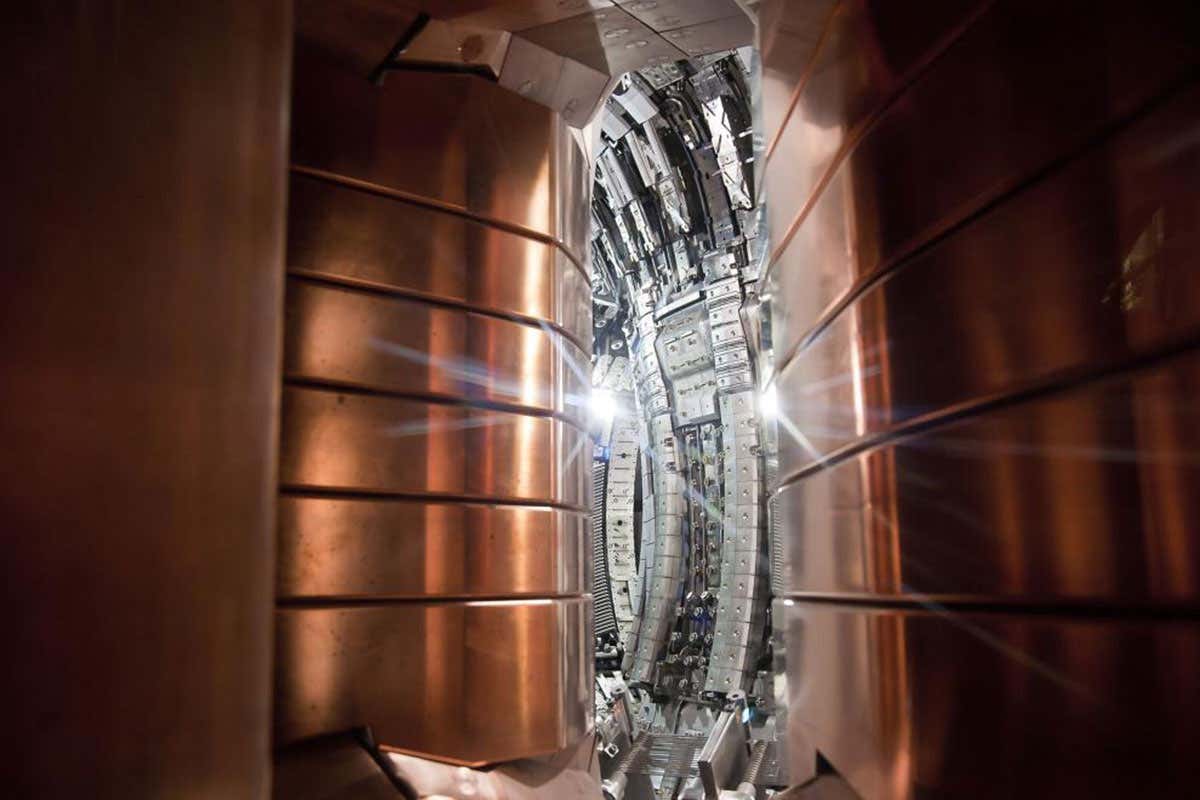
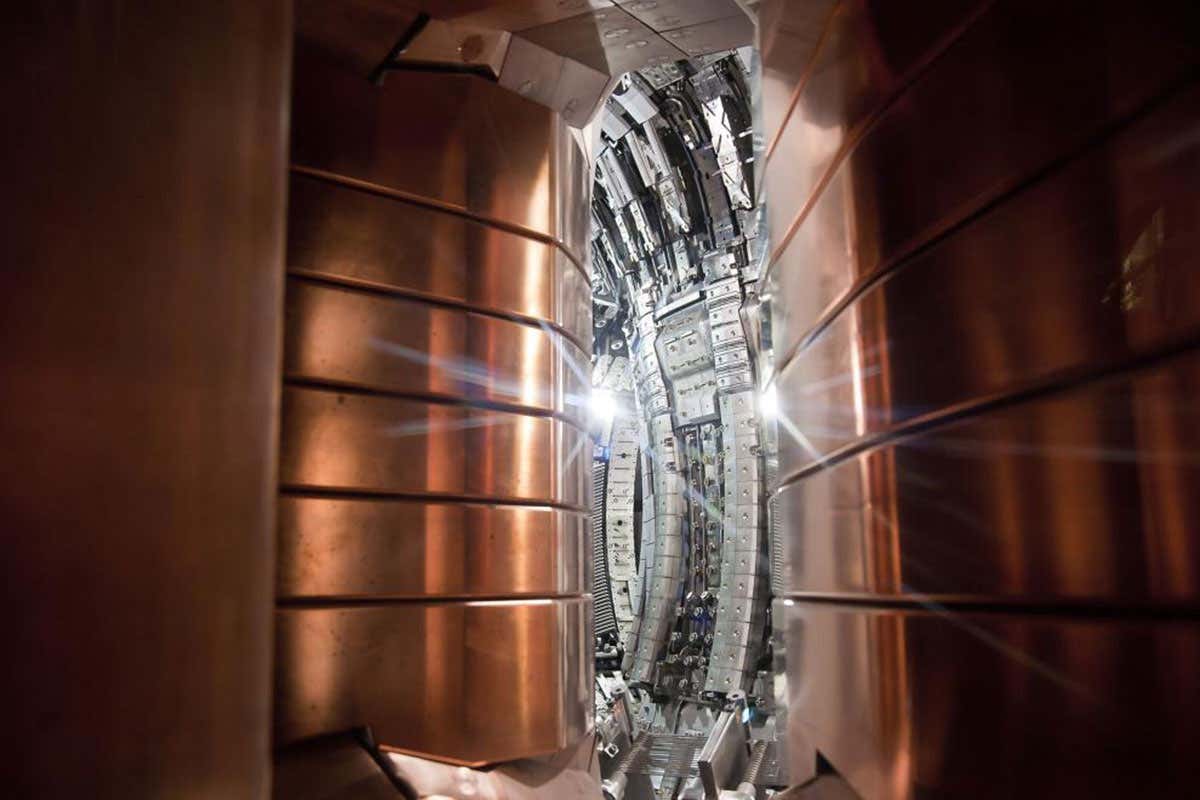
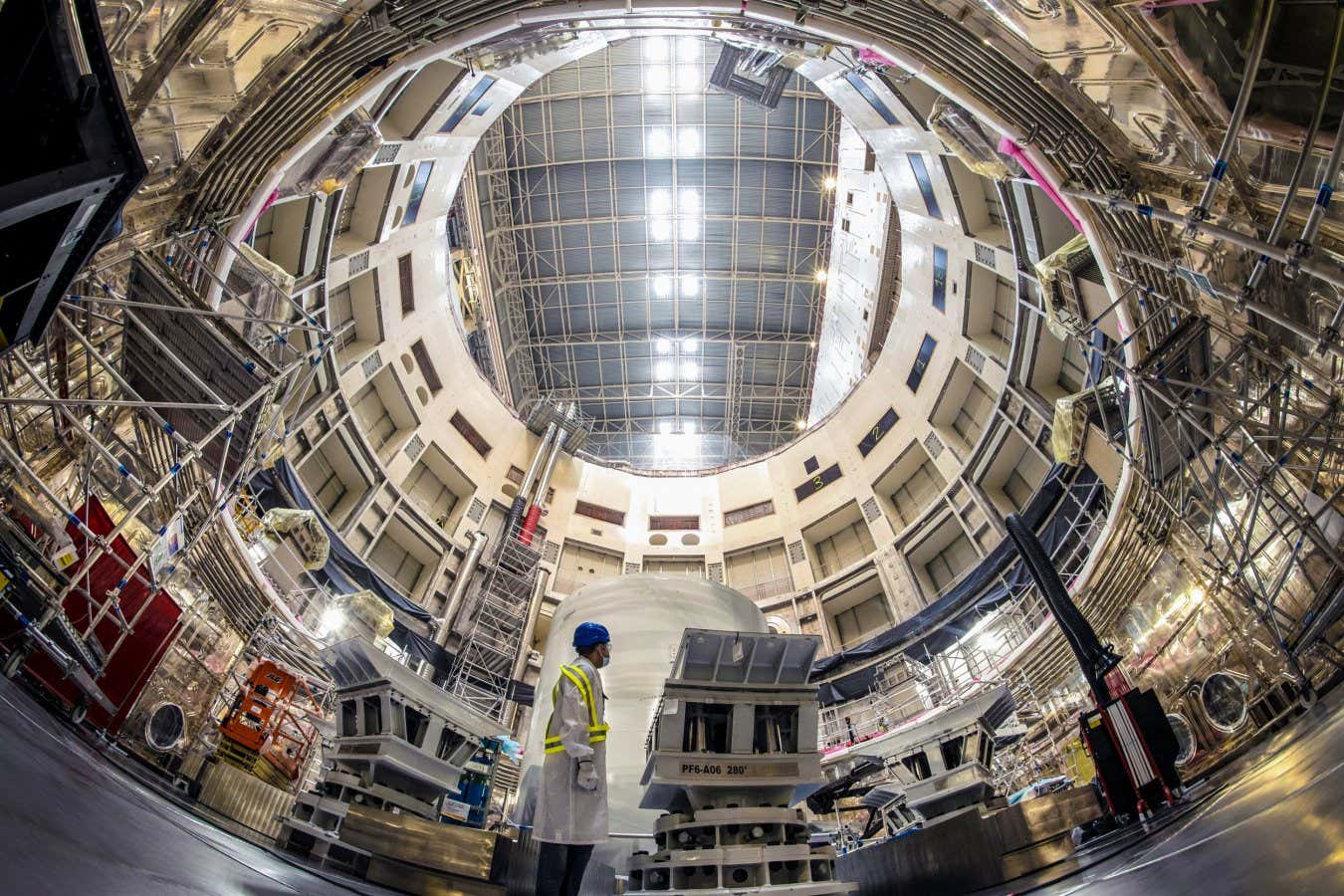
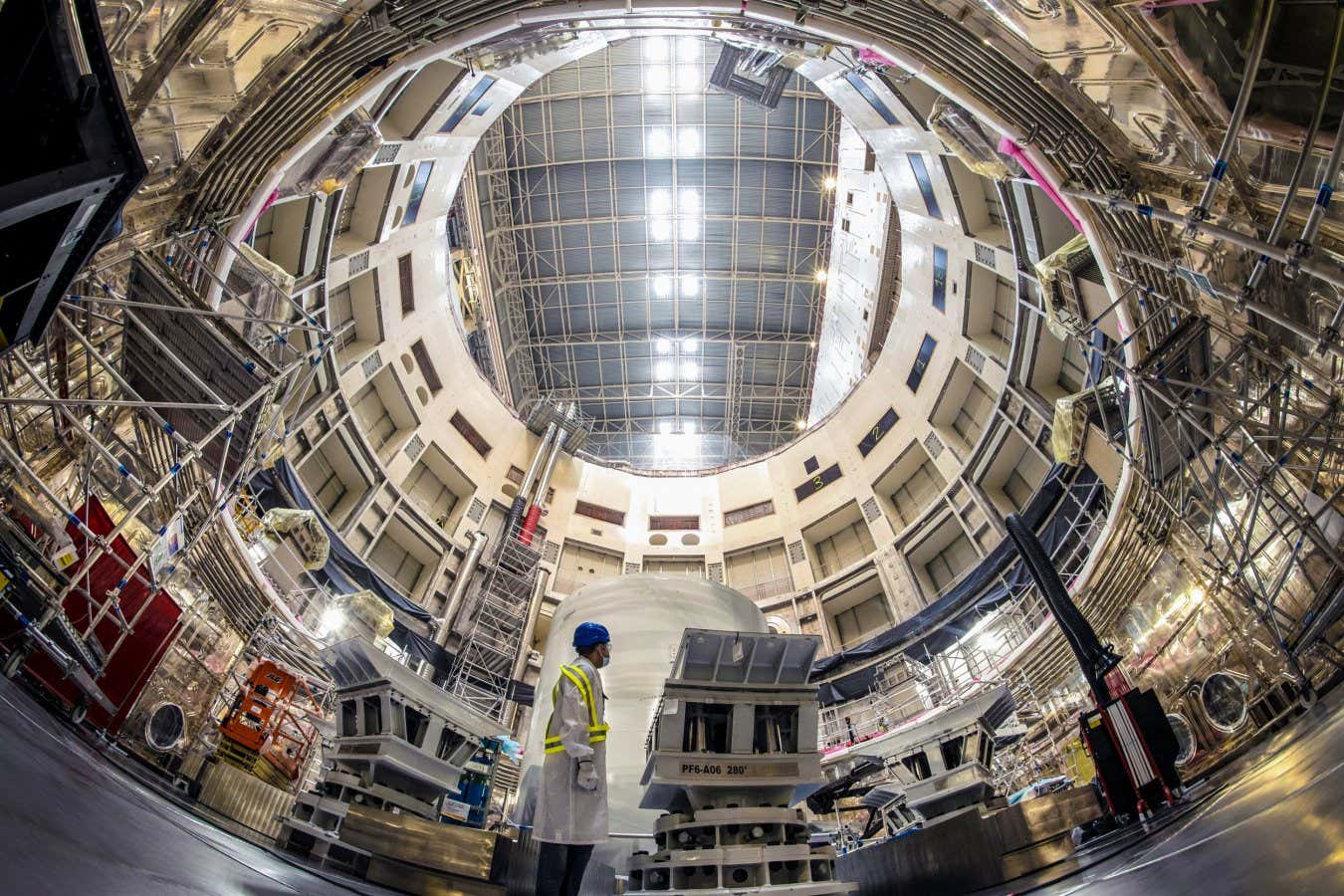
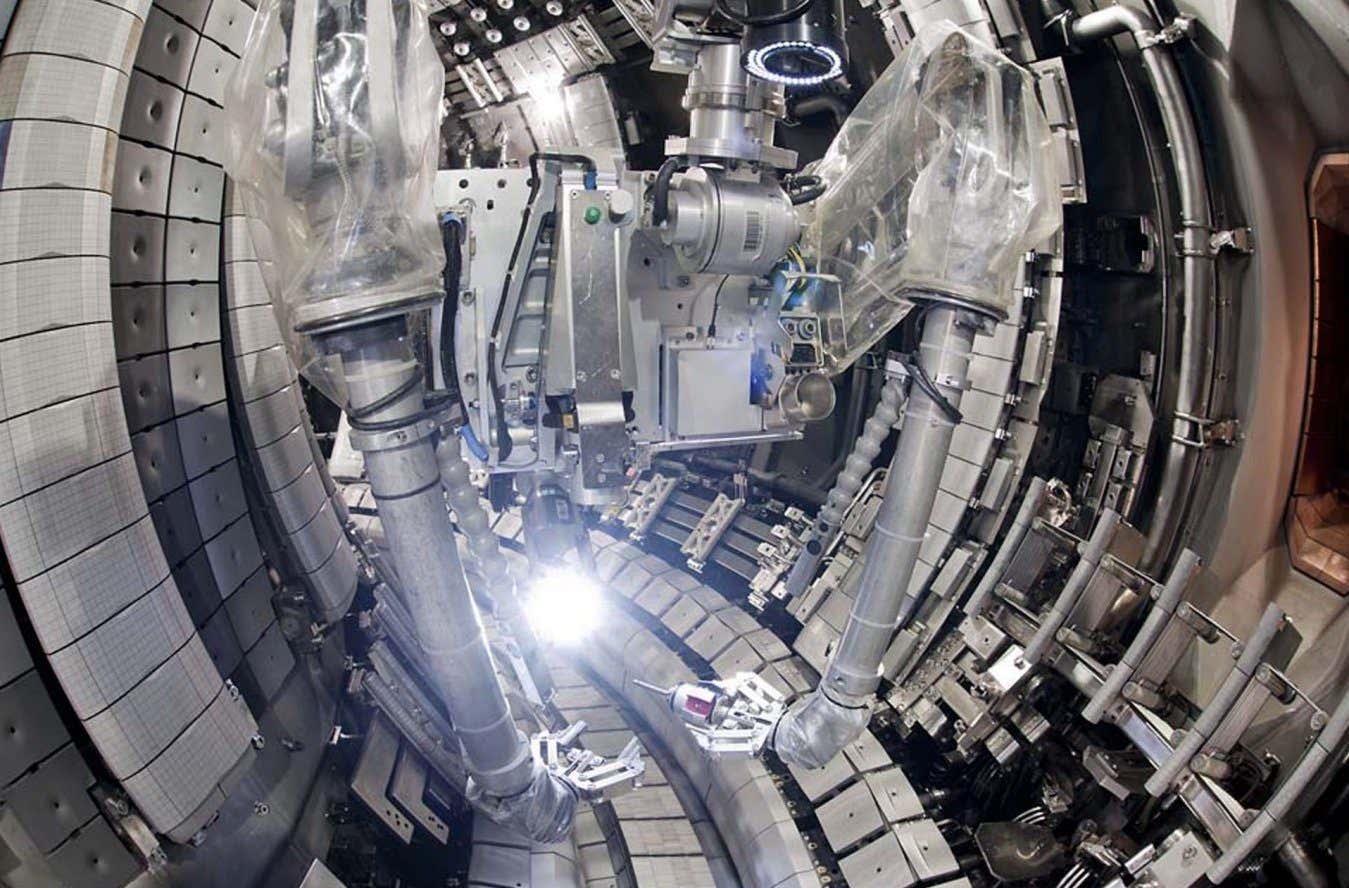
Science & Environment3 weeks agoITER: Is the world’s biggest fusion experiment dead after new delay to 2035?
-
 Science & Environment3 weeks ago
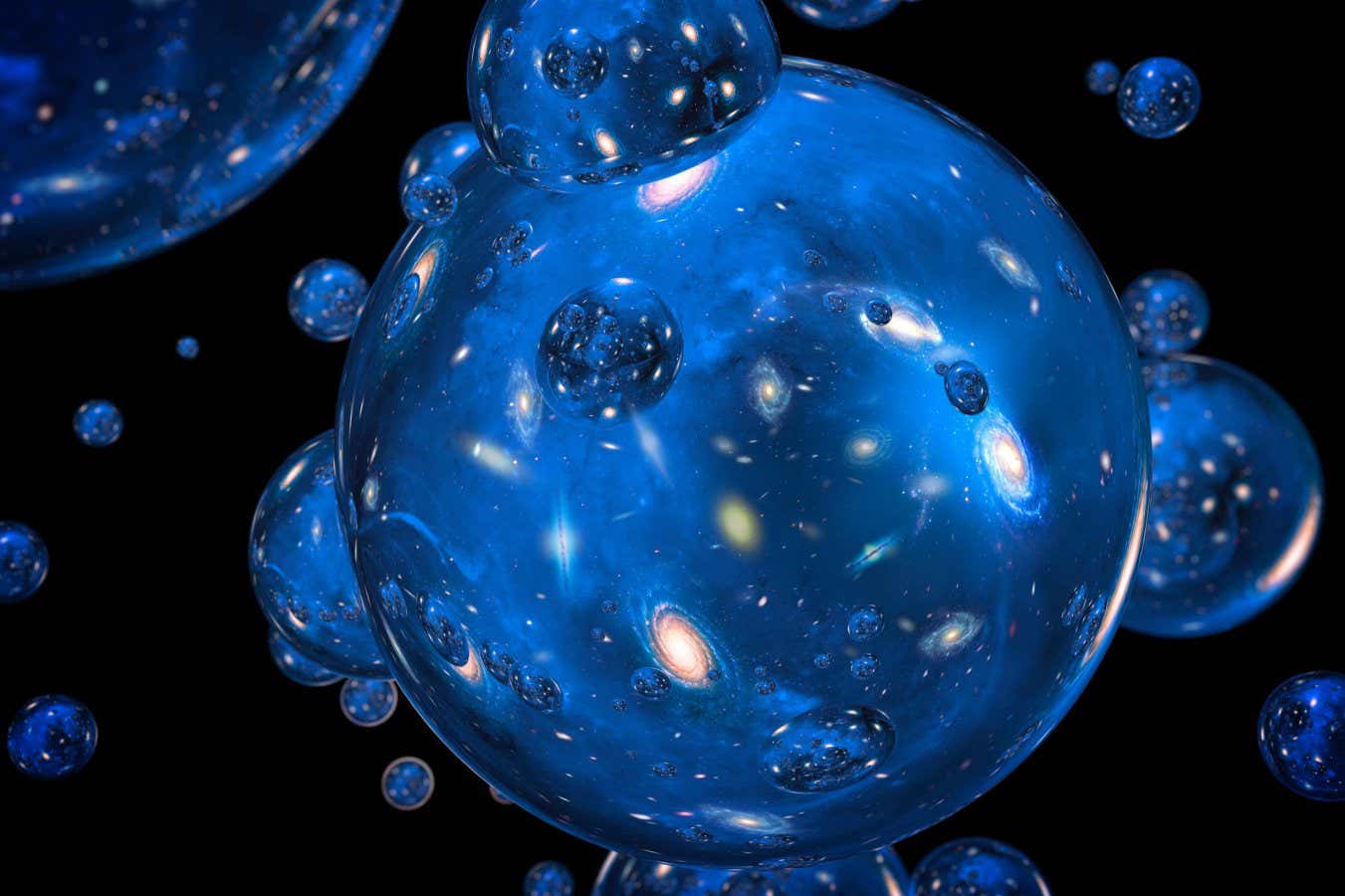
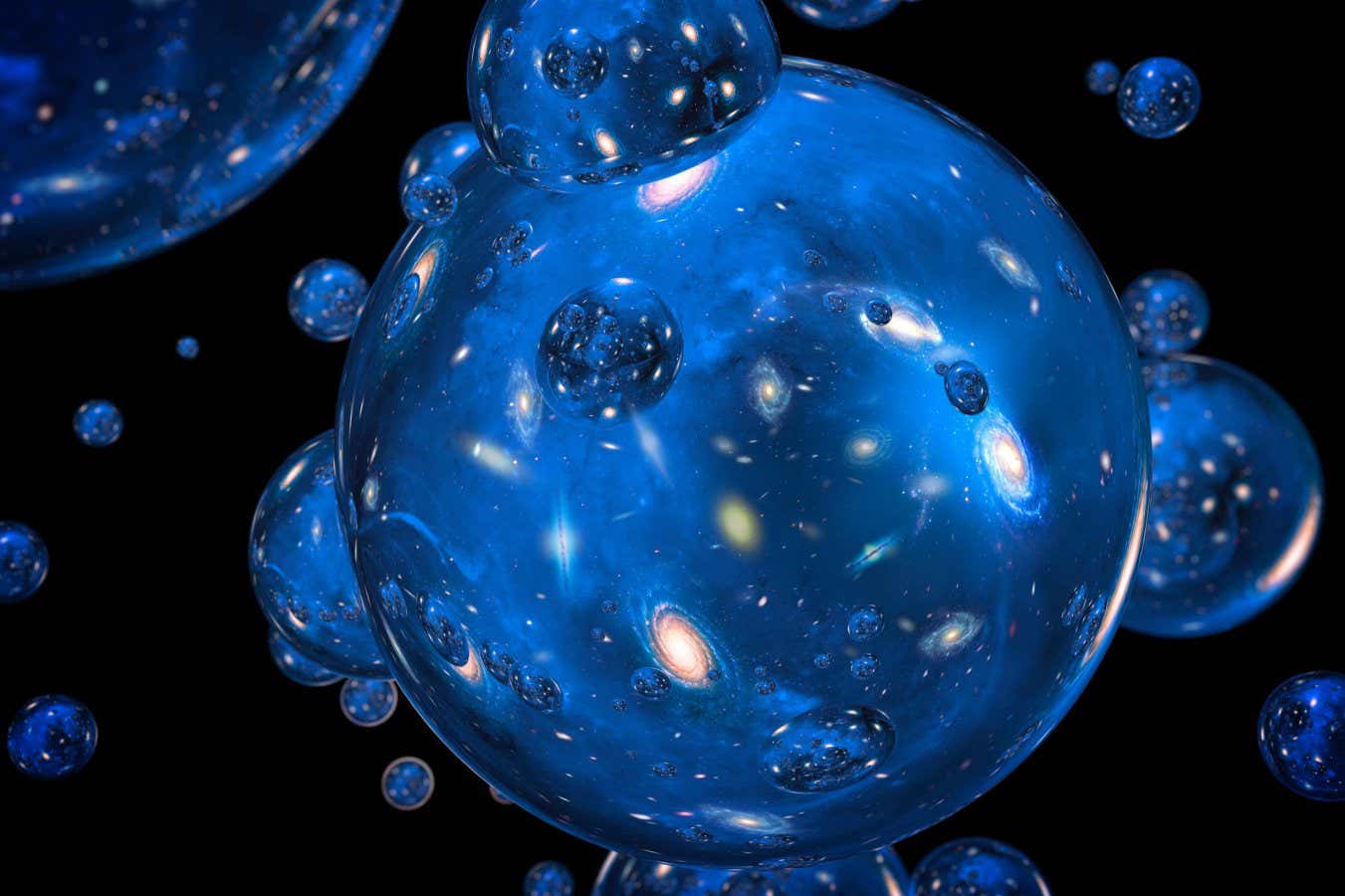
Science & Environment3 weeks agoHow to wrap your mind around the real multiverse
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoSunlight-trapping device can generate temperatures over 1000°C
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoQuantum ‘supersolid’ matter stirred using magnets
-

 News3 weeks ago
News3 weeks agoOur millionaire neighbour blocks us from using public footpath & screams at us in street.. it’s like living in a WARZONE – WordupNews
-

 Science & Environment3 weeks ago
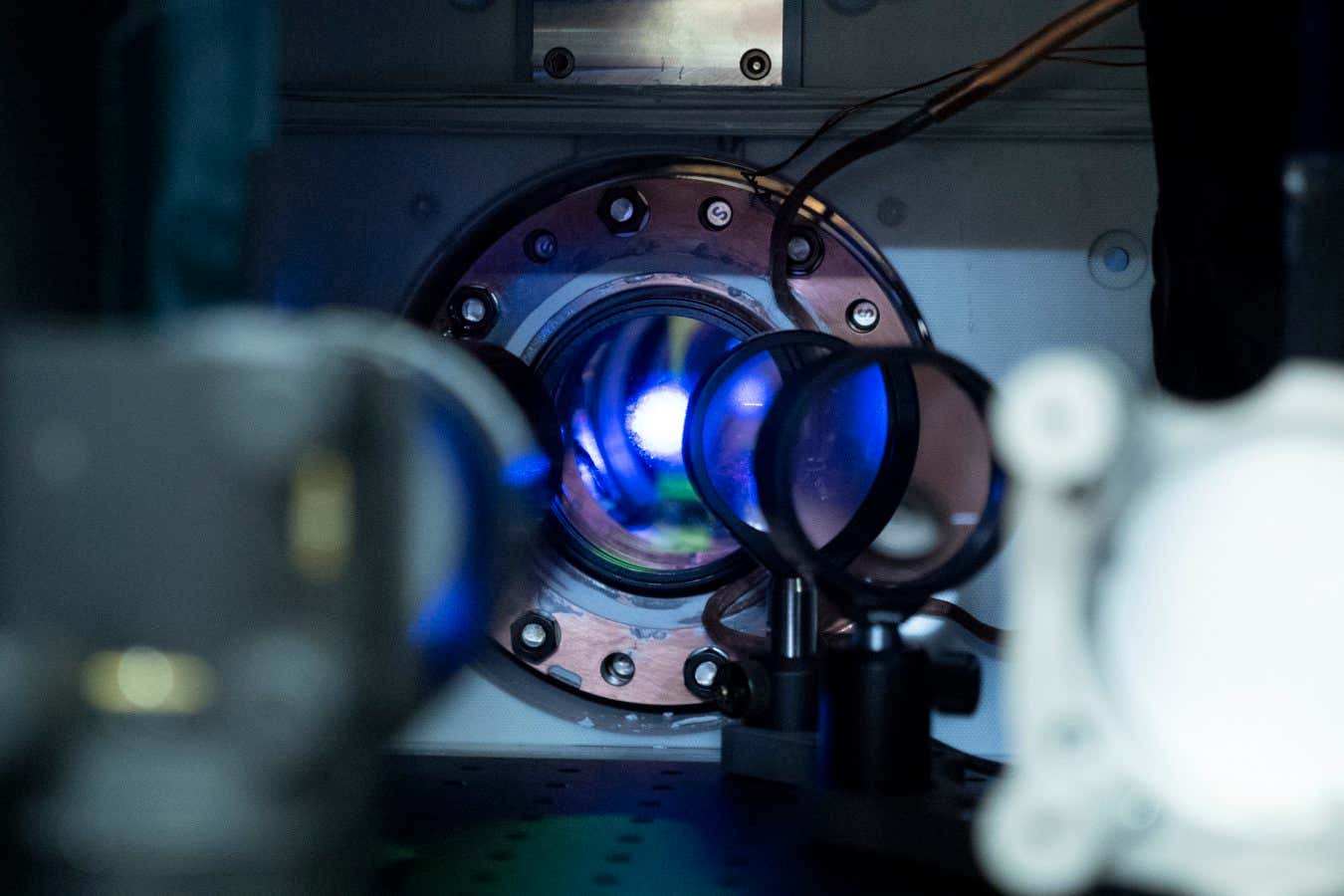
Science & Environment3 weeks agoLiquid crystals could improve quantum communication devices
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoQuantum forces used to automatically assemble tiny device
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoWhy this is a golden age for life to thrive across the universe
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoPhysicists are grappling with their own reproducibility crisis
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoTime travel sci-fi novel is a rip-roaringly good thought experiment
-
 Science & Environment3 weeks ago
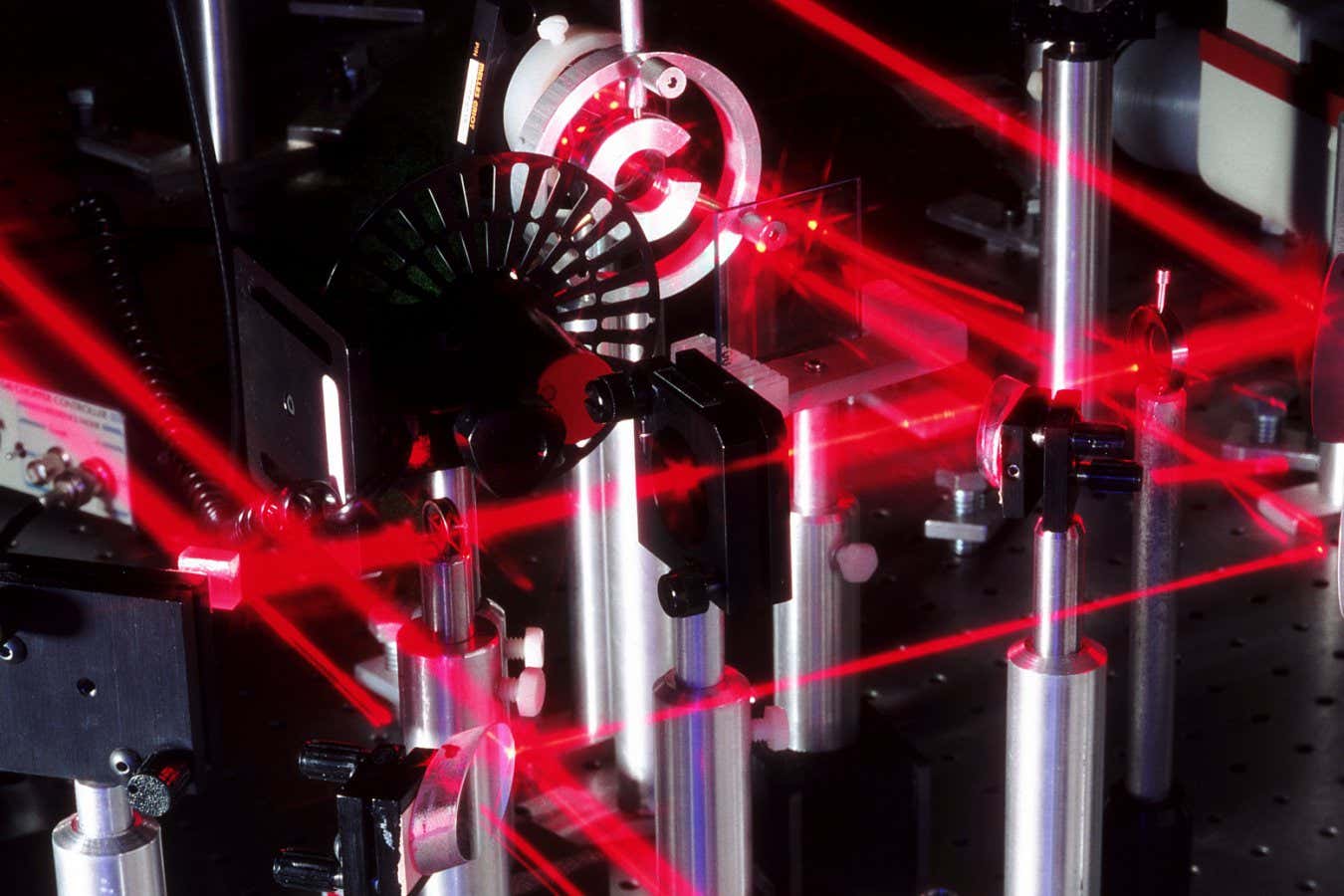
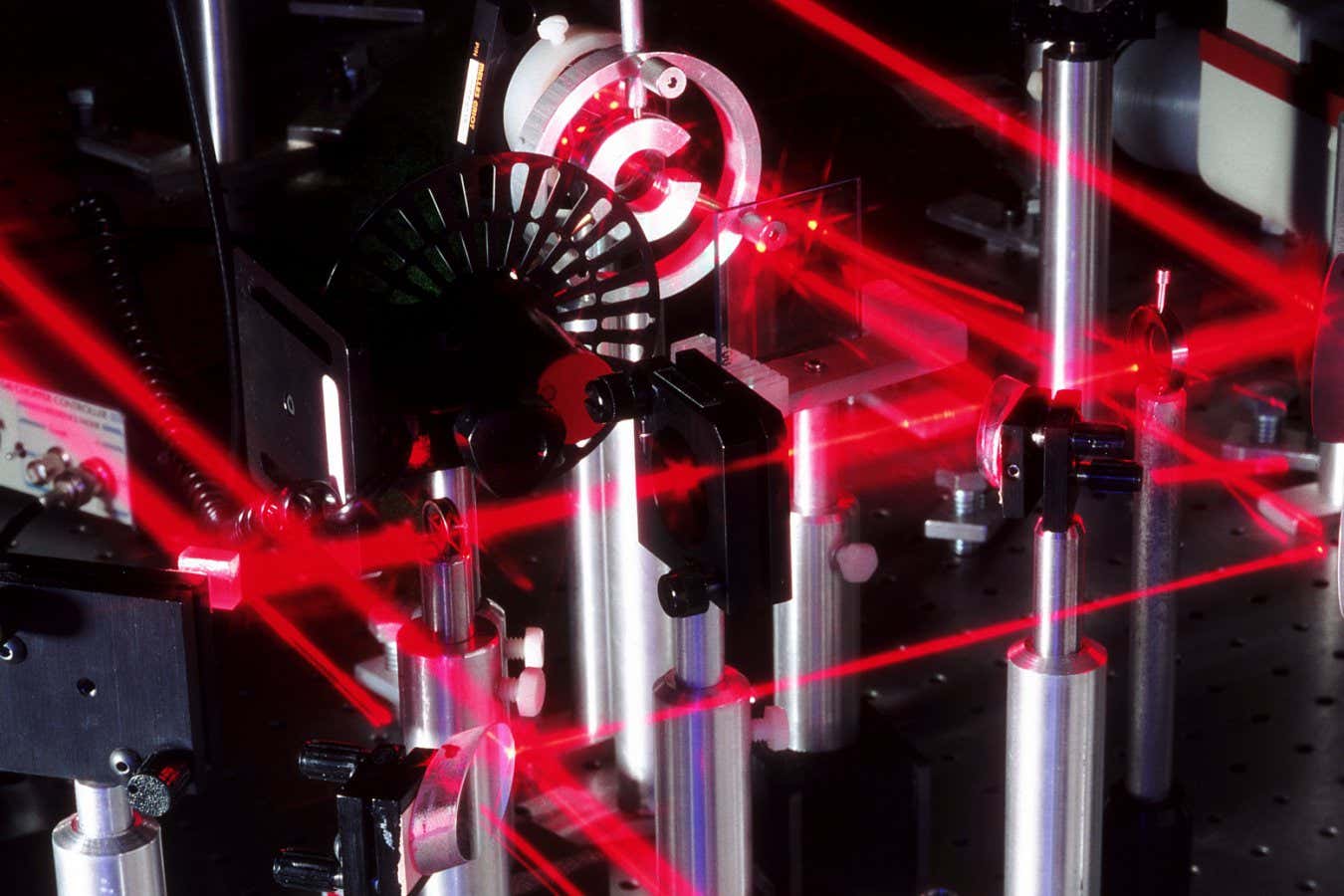
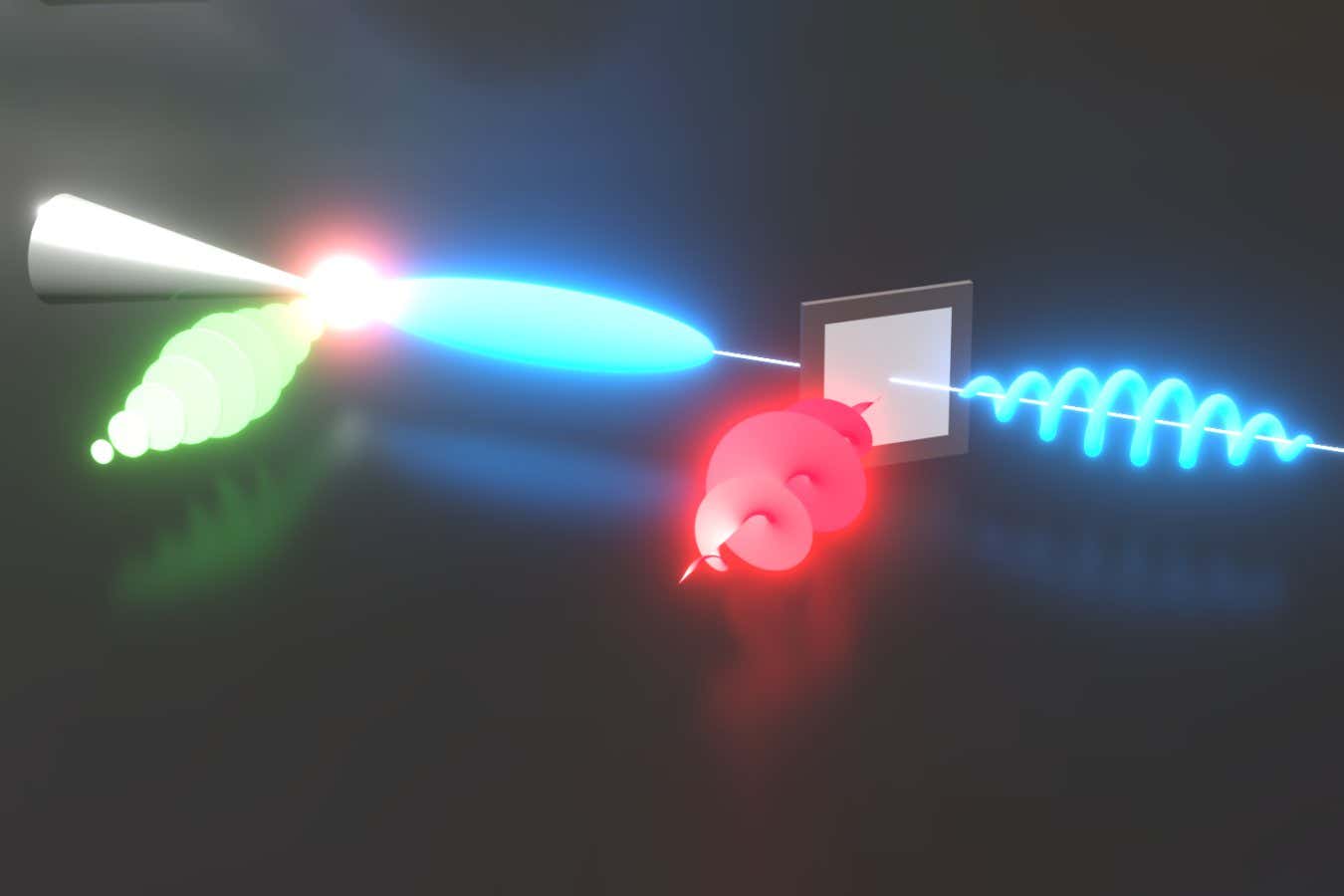
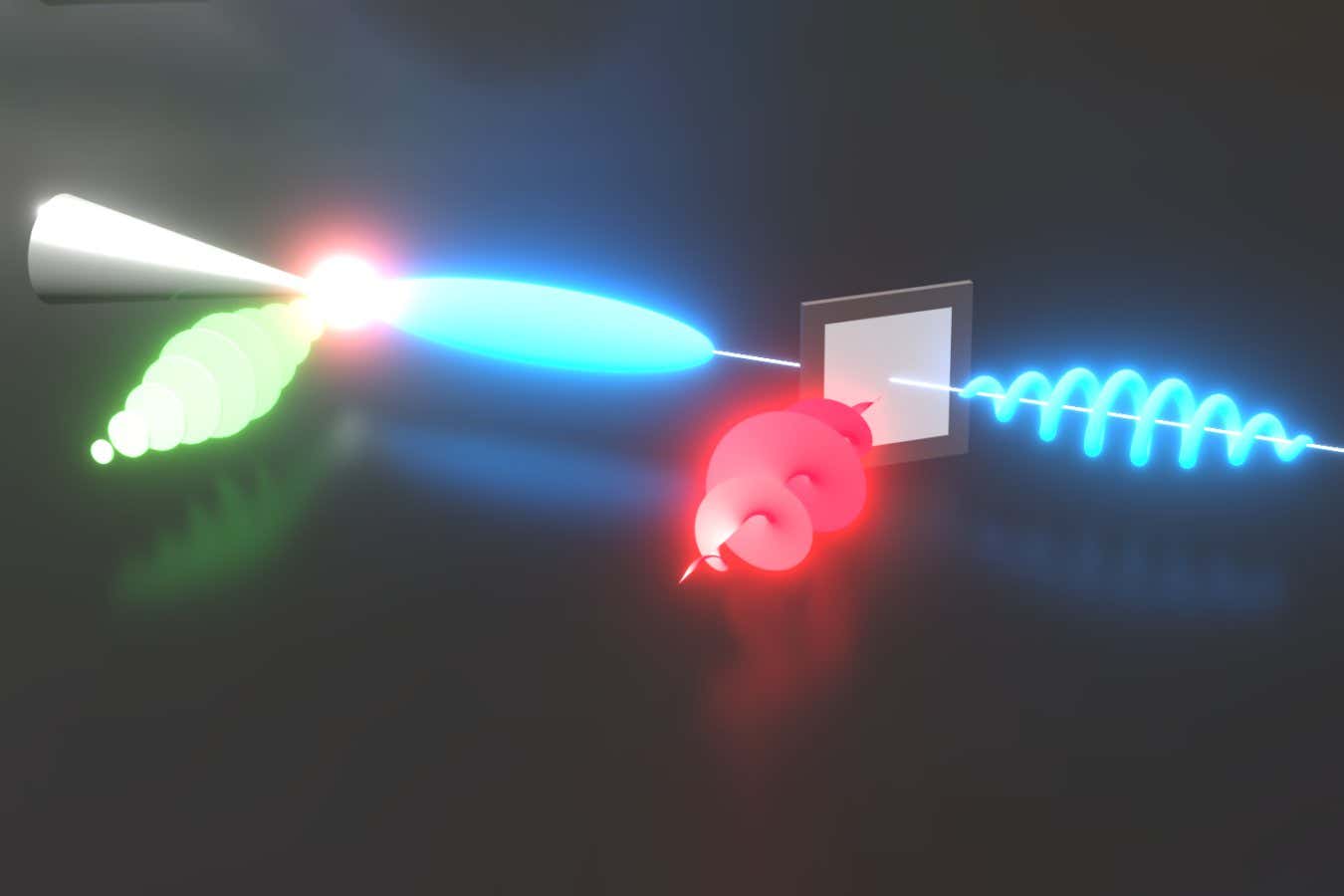
Science & Environment3 weeks agoLaser helps turn an electron into a coil of mass and charge
-

 Science & Environment3 weeks ago
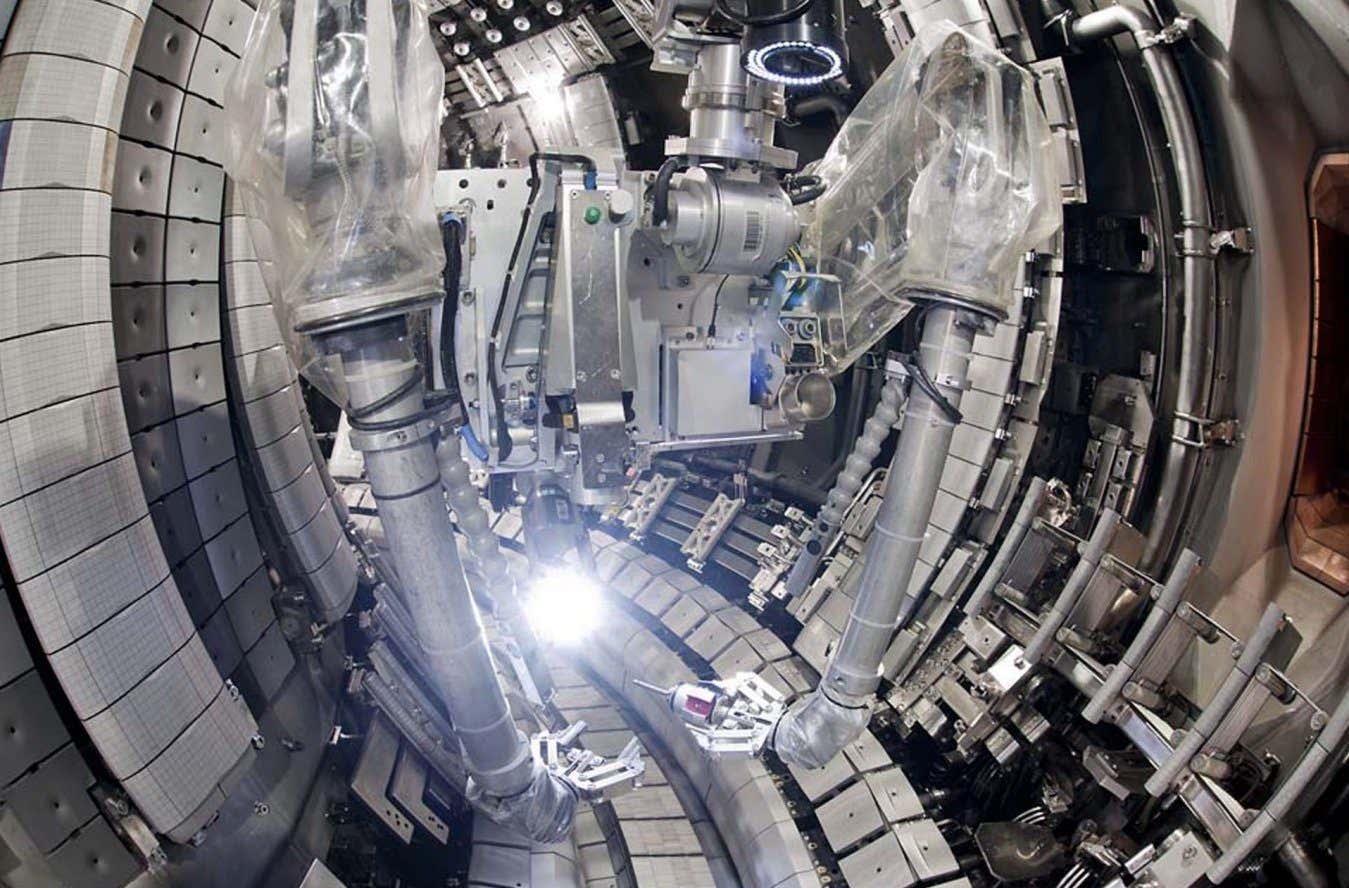
Science & Environment3 weeks agoNuclear fusion experiment overcomes two key operating hurdles
-
 Science & Environment2 weeks ago
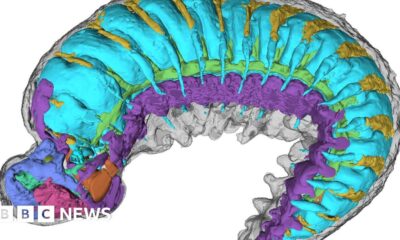
Science & Environment2 weeks agoX-rays reveal half-billion-year-old insect ancestor
-
Business2 weeks ago
Eurosceptic Andrej Babiš eyes return to power in Czech Republic
-

 News4 weeks ago
News4 weeks ago▶️ Hamas in the West Bank: Rising Support and Deadly Attacks You Might Not Know About
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoCaroline Ellison aims to duck prison sentence for role in FTX collapse
-

 News3 weeks ago
News3 weeks agoYou’re a Hypocrite, And So Am I
-

 Sport3 weeks ago
Sport3 weeks agoJoshua vs Dubois: Chris Eubank Jr says ‘AJ’ could beat Tyson Fury and any other heavyweight in the world
-
 Science & Environment3 weeks ago
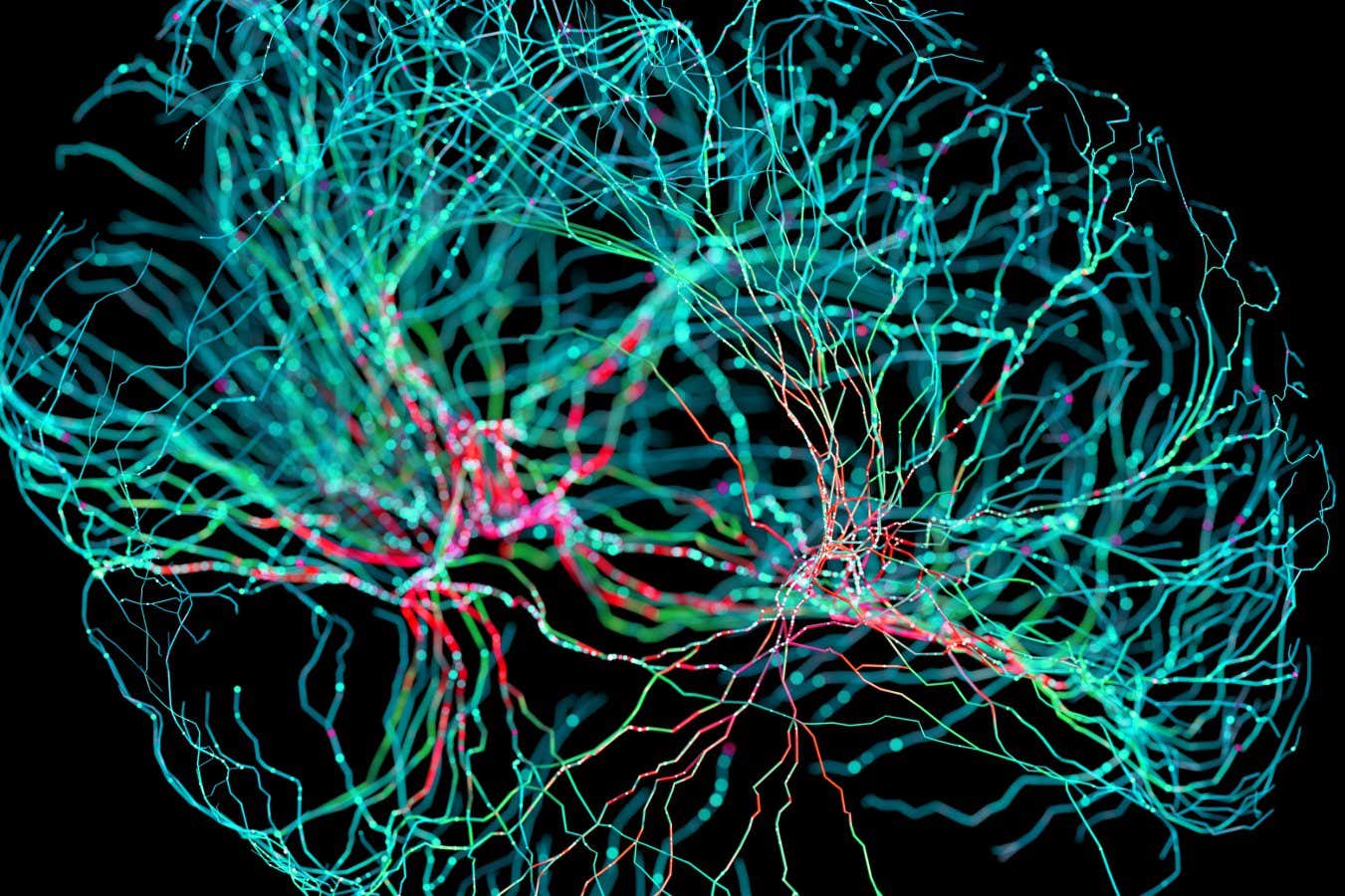
Science & Environment3 weeks agoNerve fibres in the brain could generate quantum entanglement
-

 News3 weeks ago
News3 weeks ago▶️ Media Bias: How They Spin Attack on Hezbollah and Ignore the Reality
-
 Technology2 weeks ago
Technology2 weeks ago‘From a toaster to a server’: UK startup promises 5x ‘speed up without changing a line of code’ as it plans to take on Nvidia, AMD in the generative AI battlefield
-

 Football2 weeks ago
Football2 weeks agoFootball Focus: Martin Keown on Liverpool’s Alisson Becker
-
 News3 weeks ago
News3 weeks agoNew investigation ordered into ‘doorstep murder’ of Alistair Wilson
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoA slight curve helps rocks make the biggest splash
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoRethinking space and time could let us do away with dark matter
-
Business2 weeks ago
Should London’s tax exiles head for Spain, Italy . . . or Wales?
-

 MMA2 weeks ago
MMA2 weeks agoConor McGregor challenges ‘woeful’ Belal Muhammad, tells Ilia Topuria it’s ‘on sight’
-
 Science & Environment3 weeks ago
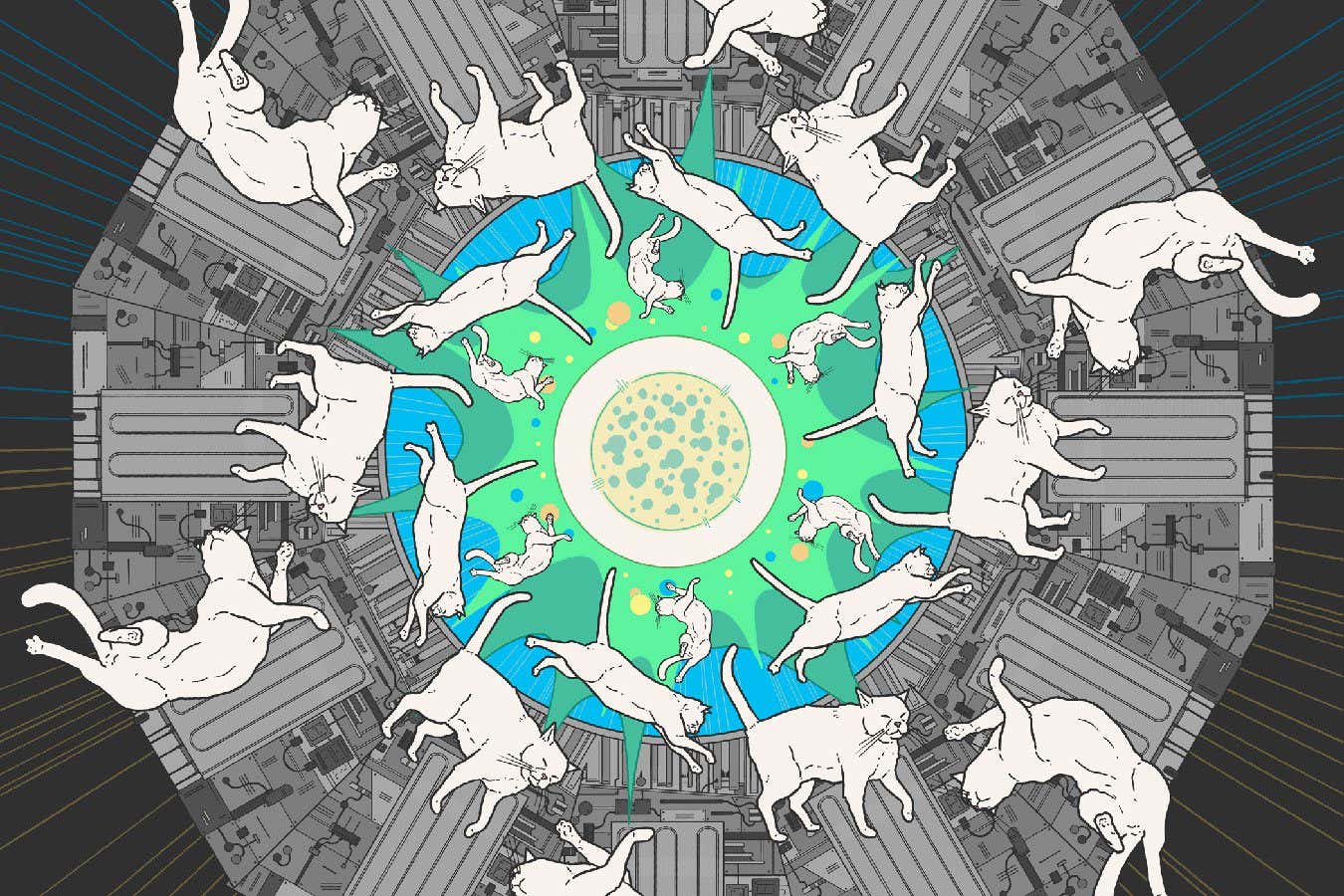
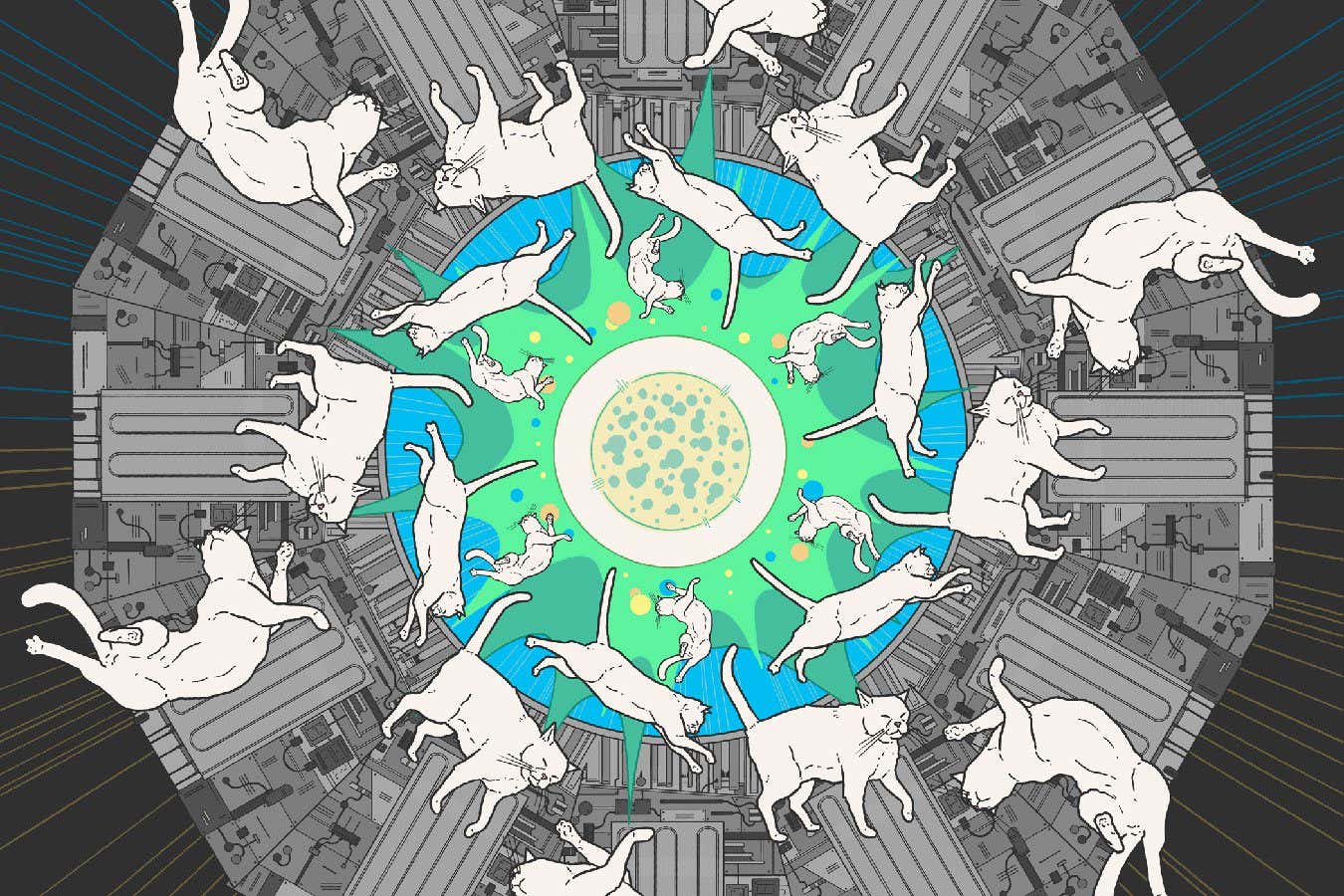
Science & Environment3 weeks agoA new kind of experiment at the Large Hadron Collider could unravel quantum reality
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoFuture of fusion: How the UK’s JET reactor paved the way for ITER
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoWhy we need to invoke philosophy to judge bizarre concepts in science
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoA tale of two mysteries: ghostly neutrinos and the proton decay puzzle
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoUK spurns European invitation to join ITER nuclear fusion project
-

 News3 weeks ago
News3 weeks agoIsrael strikes Lebanese targets as Hizbollah chief warns of ‘red lines’ crossed
-

 Technology2 weeks ago
Technology2 weeks agoIs sharing your smartphone PIN part of a healthy relationship?
-
 Technology2 weeks ago
Technology2 weeks agoQuantum computers may work better when they ignore causality
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoCardano founder to meet Argentina president Javier Milei
-
News3 weeks ago
The Project Censored Newsletter – May 2024
-

 News3 weeks ago
News3 weeks agoWhy Is Everyone Excited About These Smart Insoles?
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoMeet the world's first female male model | 7.30
-

 News3 weeks ago
News3 weeks agoFour dead & 18 injured in horror mass shooting with victims ‘caught in crossfire’ as cops hunt multiple gunmen
-

 Womens Workouts2 weeks ago
Womens Workouts2 weeks ago3 Day Full Body Toning Workout for Women
-
 Technology2 weeks ago
Technology2 weeks agoRobo-tuna reveals how foldable fins help the speedy fish manoeuvre
-

 Technology2 weeks ago
Technology2 weeks agoGet ready for Meta Connect
-

 Health & fitness2 weeks ago
Health & fitness2 weeks agoThe 7 lifestyle habits you can stop now for a slimmer face by next week
-

 Sport2 weeks ago
Sport2 weeks agoWatch UFC star deliver ‘one of the most brutal knockouts ever’ that left opponent laid spark out on the canvas
-

 Technology3 weeks ago
Technology3 weeks agoThe ‘superfood’ taking over fields in northern India
-
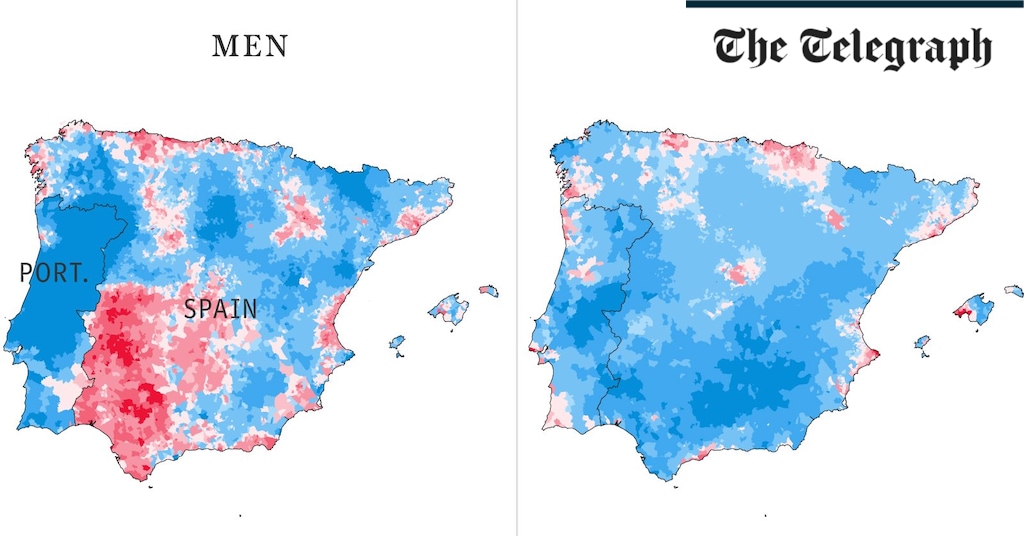
 Health & fitness3 weeks ago
Health & fitness3 weeks agoThe maps that could hold the secret to curing cancer
-

 Health & fitness3 weeks ago
Health & fitness3 weeks agoThe secret to a six pack – and how to keep your washboard abs in 2022
-

 Science & Environment3 weeks ago
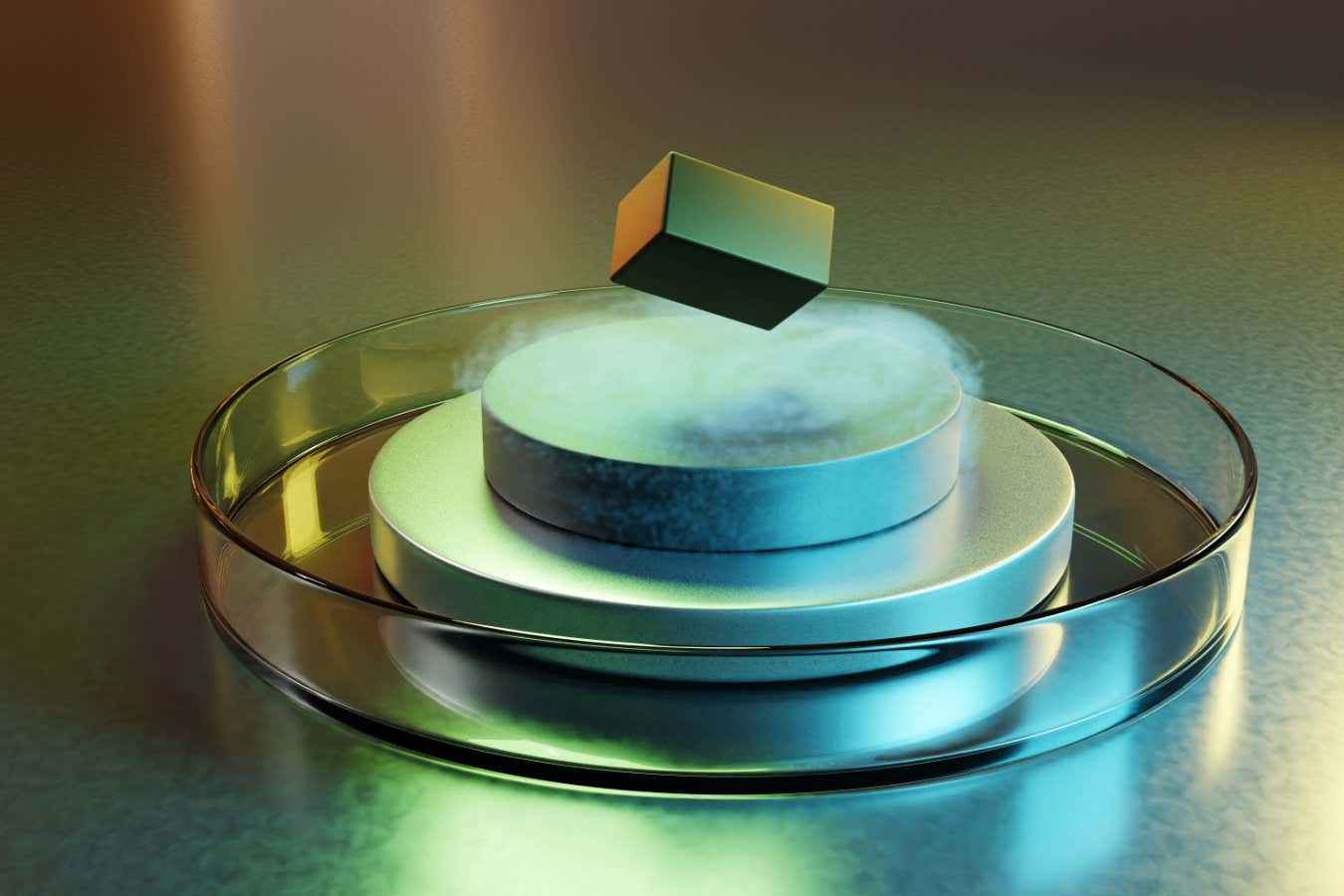
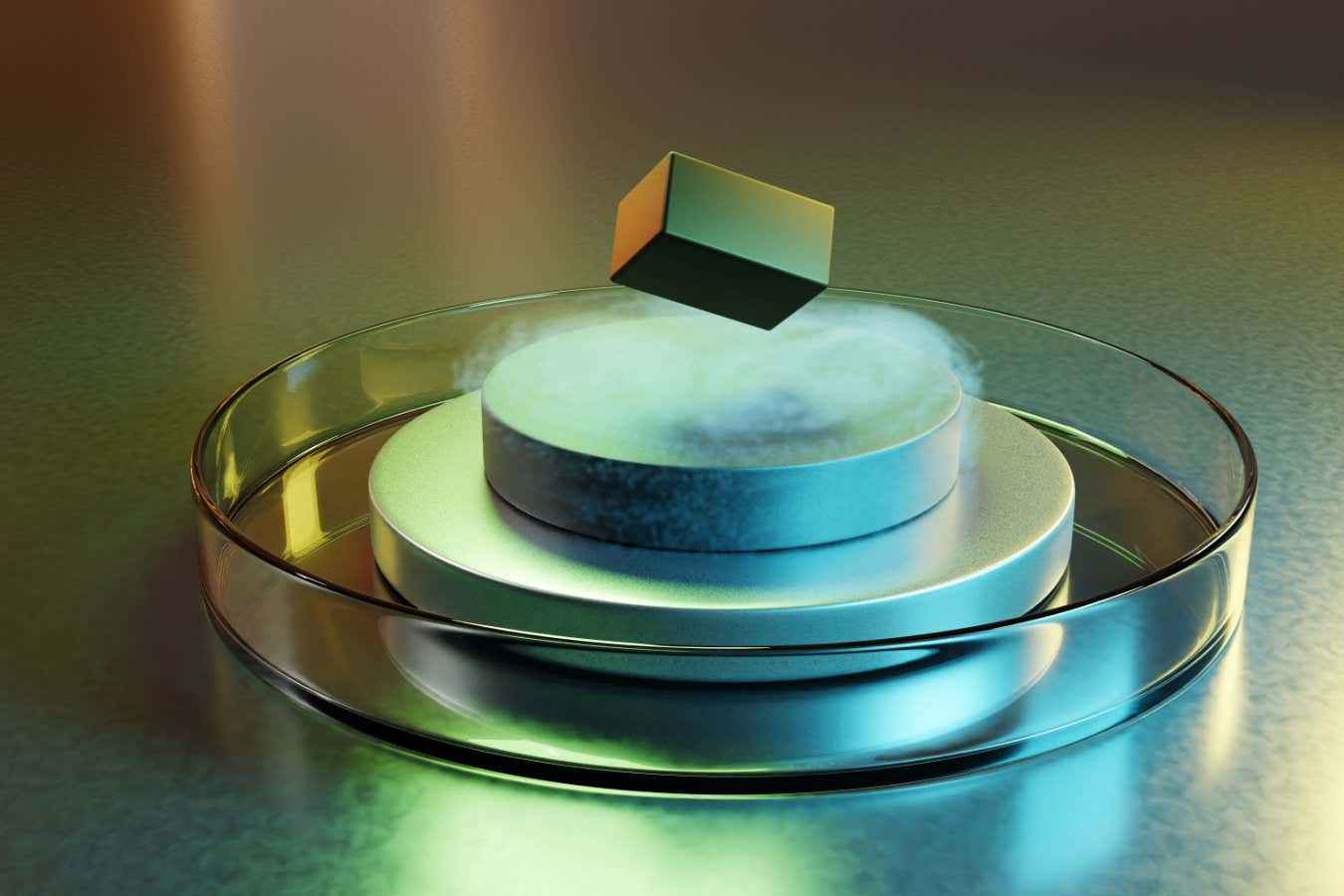
Science & Environment3 weeks agoBeing in two places at once could make a quantum battery charge faster
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoLow users, sex predators kill Korean metaverses, 3AC sues Terra: Asia Express
-
Politics3 weeks ago
UK consumer confidence falls sharply amid fears of ‘painful’ budget | Economics
-

 Womens Workouts3 weeks ago
Womens Workouts3 weeks agoBest Exercises if You Want to Build a Great Physique
-

 Womens Workouts3 weeks ago
Womens Workouts3 weeks agoEverything a Beginner Needs to Know About Squatting
-

 TV3 weeks ago
TV3 weeks agoCNN TÜRK – 🔴 Canlı Yayın ᴴᴰ – Canlı TV izle
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoCNN TÜRK – 🔴 Canlı Yayın ᴴᴰ – Canlı TV izle
-

 Servers computers2 weeks ago
Servers computers2 weeks agoWhat are the benefits of Blade servers compared to rack servers?
-
Business1 week ago
Ukraine faces its darkest hour
-
Business3 weeks ago
JPMorgan in talks to take over Apple credit card from Goldman Sachs
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoQuantum time travel: The experiment to ‘send a particle into the past’
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoHow one theory ties together everything we know about the universe
-

 News3 weeks ago
News3 weeks agoChurch same-sex split affecting bishop appointments
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoTiny magnet could help measure gravity on the quantum scale
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoBitcoin miners steamrolled after electricity thefts, exchange ‘closure’ scam: Asia Express
-
 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoDorsey’s ‘marketplace of algorithms’ could fix social media… so why hasn’t it?
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoDZ Bank partners with Boerse Stuttgart for crypto trading
-
 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoBitcoin bulls target $64K BTC price hurdle as US stocks eye new record
-

 Sport3 weeks ago
Sport3 weeks agoUFC Edmonton fight card revealed, including Brandon Moreno vs. Amir Albazi headliner
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoBlockdaemon mulls 2026 IPO: Report
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoEthereum is a 'contrarian bet' into 2025, says Bitwise exec
-

 News2 weeks ago
News2 weeks agoUS Newspapers Diluting Democratic Discourse with Political Bias
-

 Technology2 weeks ago
Technology2 weeks agoThe best robot vacuum cleaners of 2024
-

 Politics3 weeks ago
Politics3 weeks agoTrump says he will meet with Indian Prime Minister Narendra Modi next week
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoHow do you recycle a nuclear fusion reactor? We’re about to find out
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoDecentraland X account hacked, phishing scam targets MANA airdrop
-
 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoRedStone integrates first oracle price feeds on TON blockchain
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks ago‘No matter how bad it gets, there’s a lot going on with NFTs’: 24 Hours of Art, NFT Creator
-
Business3 weeks ago
Thames Water seeks extension on debt terms to avoid renationalisation
-
Business3 weeks ago
How Labour donor’s largesse tarnished government’s squeaky clean image
-
Politics3 weeks ago
‘Appalling’ rows over Sue Gray must stop, senior ministers say | Sue Gray
-

 Technology3 weeks ago
Technology3 weeks agoiPhone 15 Pro Max Camera Review: Depth and Reach
-

 News3 weeks ago
News3 weeks agoBrian Tyree Henry on voicing young Megatron, his love for villain roles
-

 News3 weeks ago
News3 weeks agoBrian Tyree Henry on voicing young Megatron, his love for villain roles
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoCoinbase’s cbBTC surges to third-largest wrapped BTC token in just one week
-

 MMA3 weeks ago
MMA3 weeks agoRankings Show: Is Umar Nurmagomedov a lock to become UFC champion?
-

 Travel2 weeks ago
Travel2 weeks agoDelta signs codeshare agreement with SAS
-

 Politics2 weeks ago
Politics2 weeks agoHope, finally? Keir Starmer’s first conference in power – podcast | News
-

 Science & Environment3 weeks ago
Science & Environment3 weeks agoPhysicists have worked out how to melt any material
-
 Science & Environment3 weeks ago
Science & Environment3 weeks agoMost accurate clock ever can tick for 40 billion years without error
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoLouisiana takes first crypto payment over Bitcoin Lightning
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoCrypto scammers orchestrate massive hack on X but barely made $8K
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoTelegram bot Banana Gun’s users drained of over $1.9M
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks agoSEC asks court for four months to produce documents for Coinbase
-

 CryptoCurrency3 weeks ago
CryptoCurrency3 weeks ago‘Silly’ to shade Ethereum, the ‘Microsoft of blockchains’ — Bitwise exec











![Brits only feel at their very best for 13 days a month, according to research. Photo released October 9 2024.A poll of 2,000 adults revealed they feel in good health for less than half the time (42 per cent) the equivalent of only 152 days a year.The rest of the time is spent with […]](https://www.thesun.co.uk/wp-content/uploads/2024/10/152-days-year-rest-time-939439172.jpg?strip=all&w=960)
You must be logged in to post a comment Login