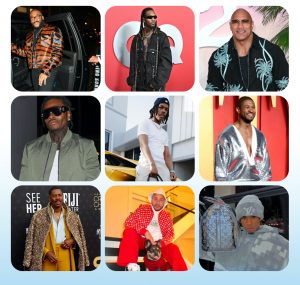
 CJ Photography Wales
CJ Photography WalesA terminally ill man was able to fulfil his dying wish to accompany his daughter down the aisle just six days before he died.
Wayne Wharton, a 61-year-old father-of-six had terminal cancer but was taken from hospital in Carmarthen to the wedding, 30 miles (48km) away in Haverfordwest, Pembrokeshire.
He was accompanied by volunteer paramedics, who stayed by his side the whole day, even sitting to eat with guests, before returning Mr Wharton to hospital.
It was one of 74 “wishes” carried out by Welsh Ambulance staff across Wales over the past five years, which allowed dying patients a final, longed-for experience.
“The paramedic pushed dad down the aisle and I held his hand,” said bride Jess Lewis, who married her partner Matthew in July last year.
“Obviously people cry at weddings because of the emotion, but every single member of the family was there and for a lot of them it was their last time to see him.
“It was a wedding but also a goodbye.”
For some, the granted wishes allowed them to use concert tickets they bought before their health declined.
But a large number just wanted a simple, final trip to the beach.
In each case, off-duty staff gave up their time.
They used non-emergency vehicles not in service on the day, to transport patients referred by their palliative team.
Jess said once her dad’s health deteriorated she was prepared to cancel the big day if her dad could not be there.
But clinicians suggested the Wish Ambulance.
“It meant the world to us, it really did,” said Wayne’s wife, Christina.
“We can’t thank them enough for what they did.”
 CJ Photography Wales
CJ Photography WalesIt is one of a number of ways the ambulance service in Wales has attempted to improve care for patients at the end of life.
Amy Prentice is part of a small team of paramedics given additional palliative care training, which focuses on symptom relief when a cure is not possible.
Her time is split between regular 999 calls and Swansea Bay’s hospital and hospice teams, who specialise in end of life care.
As a palliative care paramedic, she is part of a team making home visits to patients in their last days or weeks of life.
She said the real eye-opener has been the age of patients, adding: “We are going to people who are young.
“People in their 20s, right up to 100.
“It’s such a vast age range.”
The project, currently available across Swansea Bay and Cardiff, is the first of its kind and has meant patients can often be seen at home within hours rather than days.

In an average year, 9% of calls to the Welsh Ambulance Service have a palliative need.
But the scheme has reduced calls to both 999 and GPs, with fewer patients unnecessarily taken to A&E, prompting interest from ambulance trusts in England and Australia.
By splitting their time 50/50, it has allowed staff to keep their urgent response skills up-to-date, as well as share their palliative experience with colleagues.
“Around 90% of patients with a palliative need in Wales called 999 at some point within their last year of life,” said Ed O’Brian, the project’s clinical lead from the ambulance service.
“Statistically, they’re most likely to contact us within the last seven days of life.
“Essentially that’s a point of crisis and so it’s really important that we get those calls right.
“You can’t change the outcome – the patient is going to die, sadly.
“But you can influence a good death. You helped them in their last few hours or days of life to feel more comfortable.”

Dr Gwen Davies, clinical director for palliative care at Swansea Bay, said they had previously seen “very high rates of in-hospital deaths” where it was known patients’ preference was to die at home.
Having their own in-house paramedics changed that.
“It’s not about avoiding hospital admission,” added Dr Davies.
“It’s about making the right choice for that person.”
Ms Prentice said the training meant she was now more confident in knowing when patients can remain at home, with additional medication and support.
“If we can stop any patient dying in an ambulance outside A&E, or prevent a family watching someone deteriorate anywhere within the hospital system, I think that’s amazing,” said Ms Prentice.
“If it’s a patient’s wish to stay at home and we can facilitate that, with the right support package, you can’t measure that benefit.”
All decisions are still made in collaboration with palliative care consultants, district nurses or GPs and the option is still available for them to be taken to hospital when necessary.
Dr Margred Capel, clinical director at City Hospice in Cardiff, which also adopted the model, said patient feedback had also been positive.
“If you do have a life-threatening illness and time is running out, you don’t necessarily wish to waste time in the wrong place or spend time in A&E sitting for hours,” she said.
At a time when all budgets are tight, discussions are now taking place with the third sector to see if the scheme can be rolled out more widely.























+ There are no comments
Add yours