 Getty Images
Getty ImagesThe pressures in A&E are as bad as they were in the pandemic, NHS bosses say.
With flu cases continuing to rise and the cold weather, NHS England medical director Prof Sir Stephen Powis said hospitals were under “exceptional pressure” and facing “mammoth demand”.
He said some staff were saying the strain being placed on them felt “like some of the days we had during the height of the pandemic”.
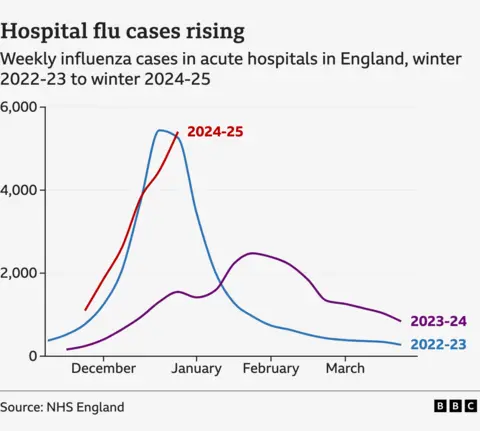
It comes as flu cases have continued to rise with the number of patients in hospital in England with the virus topping 5,400 a day on average last week – around 1,000 higher than a week before.
Around 20 NHS trusts in England have declared critical incidents this week with long delays in A&E being seen.
Problems have been seen in other parts of the UK too.
Last week the Welsh ambulance service also declared a critical incident, while in Scotland the Royal College of Emergency Medicine warned earlier this week hospitals there had become “gridlocked”.
Sir Stephen said: “It is hard to quantify how tough it is for frontline staff at the moment – with some staff working in A&E saying that their days at work feel like some of the days we had during the height of the pandemic.”
The number of patients with flu is more than three times higher than they were this time last year – and are now on par with what was seen in early 2023 – one of the worst flu seasons for many years.
The combination of bad weather and flu has meant the NHS has had a “brutal” start to the new year, according to Saffron Cordery, of NHS Providers, which represents health managers.
And she added: “We’re not out of the woods yet. Things are likely to get worse before they get better.
“Stresses and strains on emergency services are a huge concern with many patients facing long waits for ambulances and in A&Es.”
‘Like Victorian workhouse’
Liz Shearer is just one of many people who have shared their experiences with the BBC of the care being provided.
Her elderly mother spent more than 30 hours in a corridor on a hospital trolley last week because there were no bays available. She was taken to hospital after collapsing at her care home.
“I’ve never experienced anything like that in my life. It was like a Victorian workhouse. The nurses were saying how bad it is, and they were saying they just had to crack on with it.”
Yvonne Wolstenholme spent 13 hours in A&E after she was sent there by her GP because she was struggling to breathe.
“It was absolutely heaving,” she said. “Staff are snowed under, they really are rushing around like headless chickens and it’s not because of a lack of skill, it’s the lack of time to see individual patients.
“While I was there, there were at least eight ambulance crews waiting to hand over patients and obviously they are not out on the streets if they are there waiting.”
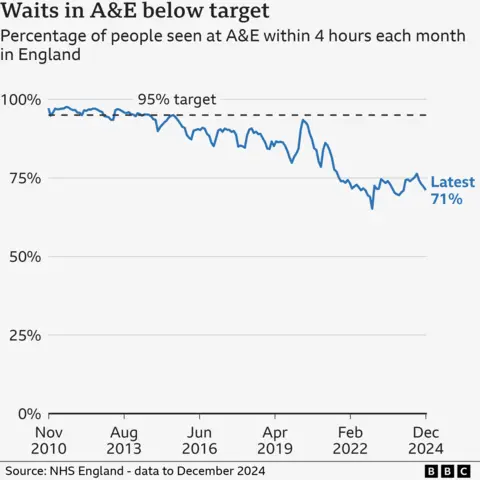
Official figures released on Thursday showed just how much the emergency care system was struggling.
- The average ambulance response time for immediately life-threatening category one calls, such as cardiac arrests, was 8 mins 40 seconds in December. The target is 7 minutes
- For category two calls, which includes heart attacks and strokes, it was 47 mins 26 seconds. The target is 18 minutes
- Just 71% of patients visiting A&E were seen and treated or admitted within the target time of four hours
But there was more positive news on routine treatment, with the hospital waiting list falling to 7.48 million at the end of November – down from 7.54 million the month before and below the record-high of 7.77 million in September 2023.
Dr Tim Cooksley, of of the Society for Acute Medicine, said the NHS was experiencing an “appalling” winter crisis.
“The reality for patients and staff is corridors full of patients experiencing degrading care, being treated in the backs of ambulances because there is simply no space in hospital and the immense physical and emotional harm that inevitably results.
“The fundamental issue is that there is a continued lack of capacity throughout the year – a tough flu season must not be used as a political excuse for the current situation.”


























+ There are no comments
Add yours